What is a Medical Biller?
A certified medical biller is a skilled medical worker who interpret medical codes and submit bills to insurance companies, patients and other agencies for medical services. The certified medical biller must be skilled in understanding medical terminology and searching the medical provider’s documentation to identify all diagnoses, conditions, reasons for treatment, services and procedures recorded, and to assign the appropriate billing code to each.
The codes determine the amount that the physician is paid for his or her services. The codes are contained in the medical records coder “bibles,” the ICD-9 and CPT-4 books. Working as a certified medical billing specialist requires a strong background not only in medical terminology, but also in anatomy and physiology, pharmacology, computer and typing skills, billing, and accounting. Source: http://www.payscale.com/research/US/Job=Certified_Medical_Billing%2FCoding_Specialist/Hourly_Rate
Online Medical Billing Course — Learn Medical Billing Online

What Does A Medical Biller Do?
Medical billers are really in charge of making sure everyone is being billed correctly. Some of this involves talking with patients and/or health insurance companies on a regular basis to make sure all invoices are paid on time. The biller should understand coding language and how to read medical invoices. This is perfect for someone who wants to have a balance of working with people (on the phone) and also spending time assessing invoices and data. Source: http://www.medicalbillingcareer.org/medical-billing-coding/
Certified medical biller work in conjunction with physicians and other medical providers and, in addition to coding services, provide education to providers regarding medical record requirements and conduct chart reviews for completeness. They have the ability to make their own schedule, and with telecommuting can even work at home. Source: http://www.payscale.com/research/US/Job=Certified_Medical_Billing%2FCoding_Specialist/Hourly_Rate
Daily tasks of a medical biller could include auditing and submitting claims for patient visits, diagnoses, and medical procedures to insurance companies, patients, and other payers. You may have to handle problems with billing. For example, you may need to make collection calls or submit claims to collection agency when bills are overdue, appeal denied claims, and process payments. You may also have to call insurance companies to get authorization for procedures in order to guarantee the claim will be paid once submitted. Source: http://learn.org/articles/What_Does_a_Medical_Biller_Do.html
So in summary, a medical biller:
- Codes billing statements
- Ensures payment
- Manages patient records
- Enters and verifies information
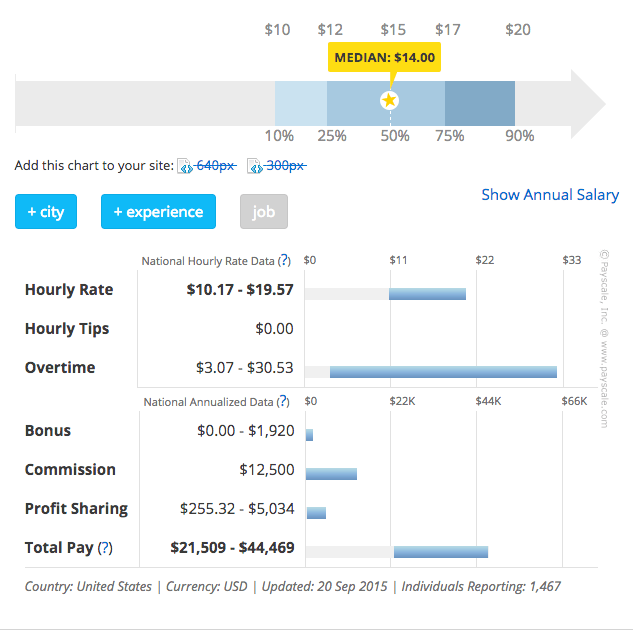
How Much Does a Certified Medical Biller make?
According to the U.S. Bureau of Labor Statistics (BLS, www.bls.gov), the employment of medical records and health information technicians, including medical billers, is expected to grow by 22% between 2012 and 2022. The BLS also reported the median annual salary earned by such specialists as $34,160 in May 2012. The Bureau notes that billing and posting clerks employed by physicians’ offices earned an average of $34,150 a year, while those who worked at hospitals averaged $34,350 annually in 2012. Source: http://learn.org/articles/What_Does_a_Medical_Biller_Do.html
In an hourly rate, the average wage for a certified medical biller is $14.69 per hour. Most people move on to other jobs if they have more than 20 years’ experience in this field. Source: http://www.payscale.com/research/US/Job=Certified_Medical_Billing%2FCoding_Specialist/Hourly_Rate
Medical Billing Certification & Training
Certification is not a requirement, but professional medical billers will find that certification leads to more job opportunities, better pay, and more chances for significant career advancement.
Certified medical biller students also complete a hands-on practicum prior to graduating. Certified medical biller programs are offered as diploma or degree programs. Upon graduation, the coder must take and pass a national certification exam.
What is the standard certification for an individual just beginning in the industry?
While there are several types of credentials that an individual can become certified in, the Certified Professional Coder (CPC) and the Certified Coding Specialist (CCS) are popular choices.
What qualifications should a certification class instructor possess?
Anyone teaching a certification course should be certified by the AAPC or AHIMA. While this is not a requirement, it is often found that certified instructors have a higher success rate when helping others prepare to earn their certification. Source: http://www.medicalbillingcareer.org/medical-billing-coding/
There are already online medical billing training courses and online medical billing certification available NOW and hence cutting you off from the staggering costs of traditional schools and boring classes. At CCO, we offer online medical billing certification course that would help you become a certified medical biller. Learn more about CCO’s online medical billing course.
![[CCO] Certification Coaching Organization LLC [CCO] Certification Coaching Organization LLC](https://www.cco.us/wp-content/uploads/2015/05/CCO-Logo-2015-d3-500px.png)
This article is informative