- Introduction
- Stages of Heart Failure in Medical Coding
- Heart Failure
- Verbiage
- HFrEF
- HFpEF
- Documentation
- Example 1
- Example 2
- Example 3
- ICD-10-CM
- Resources
Introduction
Hello, everyone. It is time for another Live with CCO. We’re on episode 87 and we’re gonna have fun tonight. You want to know why? Because we’re gonna talk about a disease process and I love to talk about the disease process. We’re going to be looking at the ICD-10 code set but that’s not all.
Stages of Heart Failure in Medical Coding
One of the things that we’re going to be talking about specifically today is we’re going to be talking about heart failure and the stages of heart failure. Thus, that’s part of the disease process. Why do you even need to know this? Because you’re probably telling yourself the provider puts all that information in the documentation. I just have to pull it out. I just have to abstract it. There’s more to it than that. It’s important that we understand the amount of diversity that’s within the disease process and tonight it’s just going to be heart failure, but within multiple different types of disease processes.
If we understand the different types, one, we can abstract quicker because we’ll know the content that we need or the verbiage that we need to be able to translate to the highest specificity. But in addition, we need to be able to educate our providers and let them know that the code set is so diverse that with pertinent information we can translate to that higher specificity. They may not realize it and therefore we can speak the same language and translate for them if we also understand the disease process. Now, that doesn’t mean that we have to go into the depth that they understand it but we have to at least have the ability to communicate and not maybe be on the same playing field, but we don’t want to be in that remedial level when they’re in the advanced. We want to be able to have common ground.

So, whenever you have the opportunity to learn more about a disease process, take advantage of that. Make sure that you look at that. Tonight, we’re going to talk about stages of heart failure. It does make a difference what stage of heart failure the patient is in connection to the proper code that you use.
Heart Failure
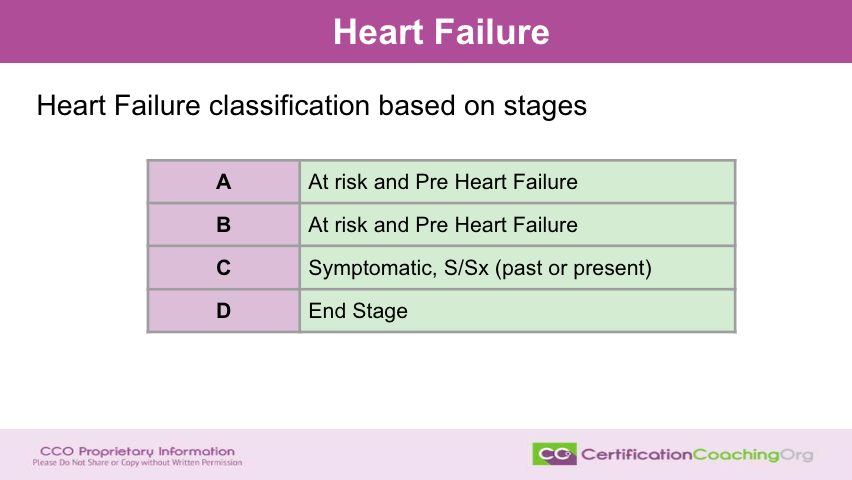
What are the different types of stages? Well, there’s A,B,C and D. How easy is that? A,B,C or D? For stage A, this is a patient that is either at risk or they are at a pre-heart failure stage. Now, that means that they’re starting to have signs and symptoms and they may even be undergoing medication or treatments to prevent the progression of the disease or to alleviate and take care of the signs and symptoms. We don’t want the disease to escalate or move forward. Now, stage B is also classified as at risk or pre heart failure. The most common stage that I see in the documentation that I look at is stage C. These are patients that are symptomatic and they have signs and symptoms whether in the past or at present. That’s important to note if the patient doesn’t have the signs and symptoms right now. That states that they had them in the past but the treatments and the medical regime that the patient is under right now has everything under good control.
Everything’s working and then you ask yourself. Why do we care as coders? Well, statistically we want to know that particular medical regime or medication, what the patients are doing is working and when we translate that documentation into a code set then it’s trackable. Right? And therefore, we can say this particular medication works very well for patients that have X, Y and Z signs and symptoms with their heart failure. They were able to alleviate those signs and symptoms or improve their quality of life due to and so again stage C is pretty common. Once the patient really starts seeing the symptoms of the disease process. Stage D is on stage. So, this is where there’s no turning back. You’re probably not going to get maybe a little alleviation of symptoms, but that the heart is progressively getting towards the heart failure stage.
Again, the stage kind of is self-explanatory. It’s probably a good point to bring up right now that in this presentation I’ve used a lot of abbreviations. I’m expecting that you already know what these abbreviations are, especially if they’re part of disease processes like CAD, hypertension and so forth. But if you don’t, just know that you can always pause and take a moment to look it up again. If you don’t know then you need to rewrite that down in your notebook and do some research on the side. Feel free to ask your colleagues, peers or other students or your instructors on what some of this verbiage is if you don’t know. but it is also a learning opportunity what you don’t understand or don’t know have that notebook and write it down so that we can come back and and reflect on that and maybe unpack something.
Verbiage
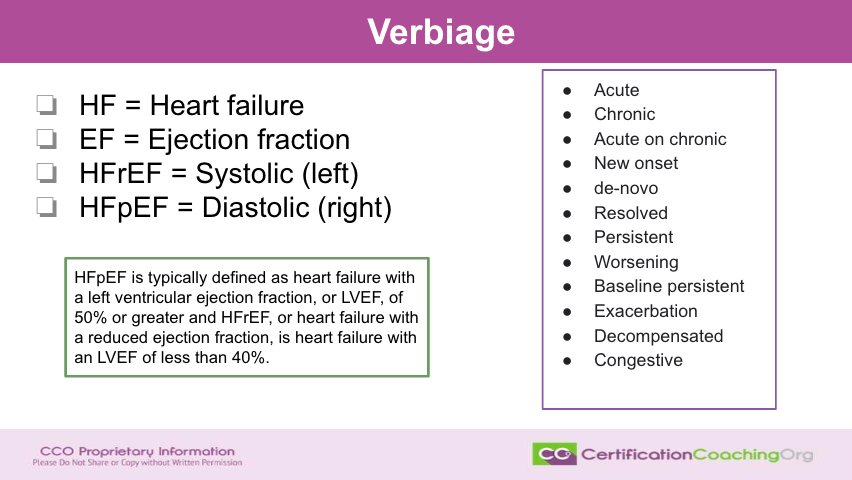
All right, let’s move forward. Let’s talk about the verbiage that you need to be familiar with. And that was a perfect segue right when we struggled most of the time with coding, it is because we don’t understand the verbiage or the verbiage wasn’t given to us in the documentation to be able to translate it at the highest specificity. Therefore, we want to have a high level of knowledge of the verbiage that’s in the disease process. So, when you see HF, that’s gonna stand for heart failure. When you see EF, that stands for ejection fraction. There’s two types of heart failure that are very commonly seen. It’s going to be systolic which is the left side of the heart and you will see that documented a lot by the provider as HFrEF so that’d be the left side of the heart is failing not being able to do its job sufficiently and that’s referred to with that little r, HFrEF.
Likewise for the right side of the heart that’s considered diastolic and that is EF little p. No, excuse me. HFpEF. Again, you see this kind of an acronym created and documented frequently. I even have a little note behind my computer that I can just look up real quick and reference because even I forget which is the left side of the heart, which is the right side of the heart when I’m looking at the Cardiology reports and the systolic and the diastolic and and everything. So, make yourself a little cheat sheet and pin at some place. The more often you look at it, the more likely that you will be able to retain that information.
So, some other verbiage that you’re going to see in the documentation that you need to be linking with heart failure is going to be the terms acute and chronic. Now, we know what a cute and chronic stand for but there’s also acute on chronic. That means the patient has chronic heart failure or CHF, but they’re having an acute episode. And then also the term new onset, you will often see that documented as new onset or acute. Again. it kind of means the same thing but it’s whichever the provider prefers to use in their documentation. There is the day Novo. There’s also resolved persistent worsening, baseline persistent exacerbation, decompensated and congestive. If there’s any of the verbiage there that you don’t feel comfortable with say if you couldn’t give a you know, a real quick elevator pitch as a description is what this is then you need to look that up.
Now, I put in the green box a little more information regarding what the heart failure areas were where it says the, excuse me. I’m not gonna say the acronym. I’m just going to say the diastolic heart failure is typically defined as heart failure with the left ventricle ejection fraction, EF, or LVEF of 50% or greater and that the systolic and then or heart failure with reduced ejection fraction is heart failure with and LVEF of less than 40%. Do you need to know this? Do you need to have this memorized? Absolutely not. Now, if you’re gonna be working in cardiology a lot then yeah you may have that but what is going to be beneficial to you is if you have documentation and you know, I50.9 has been pulled for CHF, but you know, they went in and they have these studies done and you can see the results.

Now, you could query the provider in a proper way based on what you found and you can pull into that query that, you know, the ejection fraction is at, you know, 60% per the study dah-dah-dah-dah and give that to provider so that they don’t have to go search for that information for that patient. Right? If you understand where you can pull it and give it to them then you’re going to get a reply in a more timely manner. And also, this not only saves time for communication for you and the provider used in a proper query which we won’t be talking about tonight, but, it also helps the provider save time and it shows the provider that you understand the process, right? You’re not just nagging them with a verbiage that they think maybe you don’t actually understand because surprisingly there’s a lot out there. A lot of times out there when this happens.
I’m seeing Belinda said “would you consider systolic dysfunction same as systolic heart failure”? Well, knock on wood, however, the best practice Belinda is to check with the provider if you are able to do so. Okay? Now, I know not everybody can do that. Like if you’re doing risk adjustment and it’s for an MA plan, you know, you can’t but whenever you see the word dysfunction, usually that’s going to link to heart failure, but it doesn’t have to. So, best practice for the policy for your office or for what entity you’re working for is sit down in a meeting and say all right, I see that we have the documentation of, you know, left-sided dysfunction or however you worded that and then or just a solid dysfunction and say whenever I see that am I allowed to translate that as systolic heart failure and if the provider states yes, that’s what I mean or no not all the time. Then what you do is you put your policy in place and you all agree to educate internally to decide what you’re going to do when you see that documentation.
Again, you can’t always do that. But if you check with whoever you’re coding for and say, all right, I see this. I’m making, you don’t want to use the same assumption or they like to make little verbiage jokes about that. But say, you know, I consider systolic dysfunction the same as systolic heart failure. Do you agree and if they say yes, okay, then we’re all gonna practice that but if they say no then again, you all need the same page, right? So, hopefully that answered your question. Deanna said, “I know where I work we have a query. It says systolic or diastolic dysfunction”. That’s correct, and there’s actually more information that could be put in place for that, but you’re right. We have to query open-ended. We’re not going to get into the discussion of queries. So, because that is another whole lecture. Shamika says “would you do a video on Nephrology”? Yeah, we can do that. You know I could.
HFrEF
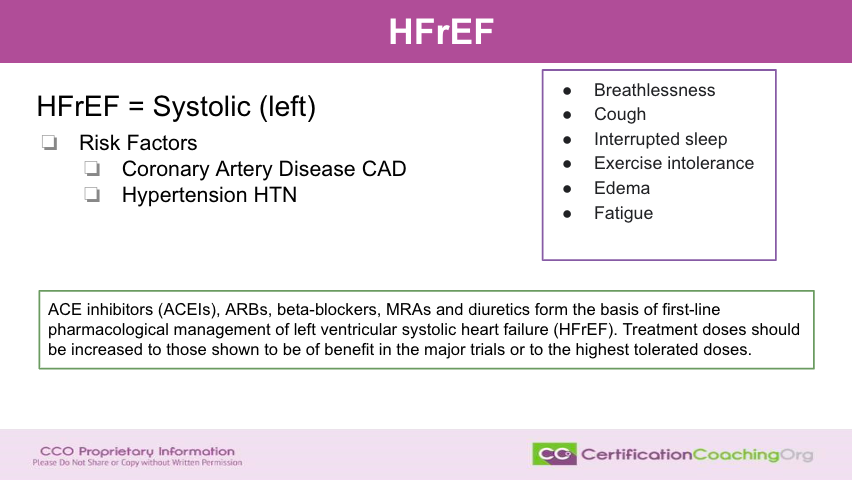
Okay. So, let’s talk a little more about the different types. For systolic left again, that’s going to be the little r so we have heart failure HF little r and then ejection fraction. What are the risk factors? Most of the time the patient has CAD or they have hypertension, but you will often see signs and symptoms. They have breathlessness. They have a cough. They aren’t able to sleep well, they have interrupted sleep. They have exercise intolerance. And then, they’ll have edema and often fatigue. Well, what do they do to treat these symptoms or the systolic or left-sided heart failure? A lot of times they’ll put them on ACE inhibitors. They can do a little bit. They usually just treat the signs and symptoms and hopefully they can maintain and not get worse. They can improve over time depending on the nature of the level of the damage that may already have been done.
There’s ARBs, beta blockers, MRAs. And again, there’s a lot of information here but that first line of defense to help with systolic heart failure is to work with medications. And then, when the patient is not doing well, they’ll work with titrating and and try to adjust doors and stuff. But they, I think, from what I’ve read is that people can build up intolerances and there could be other disease processes. Processes that are involved where some people might not be able to take this medication and so on and so forth.
There are some lifestyle changes, basic lifestyle changes involved there but systolic or left-sided heart failure is a little bit different than right-sided. So, let’s see what the differences between the two are.
HFpEF
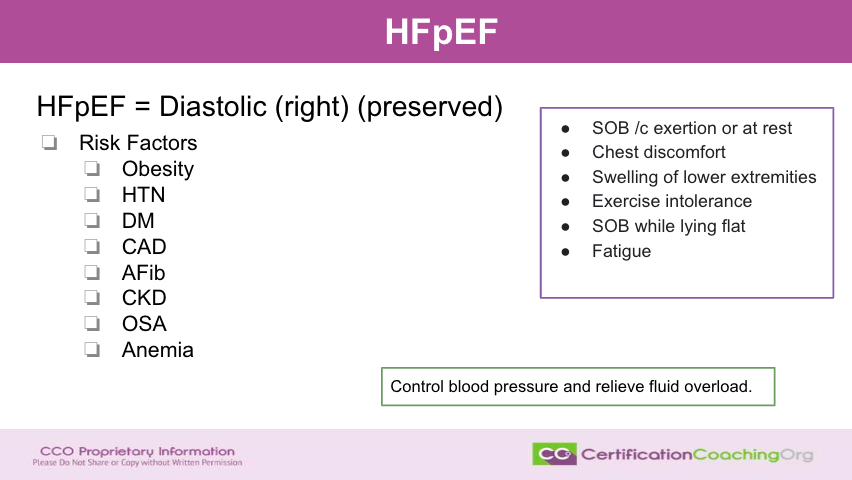
When you have a diastolic, the HF heart failure little p EF ejection fraction, this is called right or preserved. That’s why you get that little pay. The risk factors with it, we have a lot of risk factors. We have obesity and again obesity tends to be one of those really common risk factors across the board. You have hypertension, diabetes, CAD, which is coronary artery is atrial fibrillation CKD obstructive. Sleep apnea will be seen also and anemia. All of those end up being risk factors.
Now, what are the signs and symptoms? You’ll notice some of the same but shortness of breath with exertion or at rest. So, a person walks across the room and they’re short of breath or they’re sitting on their recliner with their feet up and they’re short of breath, right? So, they could have it both. They have chest discomfort. Sometimes, they can’t really explain what it is. But, it’s uncomfortable. Swelling of the lower extremities with, again, edema is that swelling but the lower extremities when you get into the diastolic heart failure you really see that extremely common and tract by the providers every time the patient comes in.
Exercise intolerance. They just can’t manage exercise. The shortness of breath while lying flat. That’s another really big telltale sign of the progression of the disease process and fatigue. They’re just worn out. The heart is not working as well. So, what did they do to control this? Actually, controlling the blood pressure and taking care of the fluid overload that edema. So, they’ll give them the blood pressure medications and they’ll be put on a diuretic to get rid of all of that excess fluid and that gives them a lot of comfort in the chest. Let’s see. Let me check. Deanna says I know where I work. We have a query we looked at that one. Belinda says it sounds like best not to pick it up. Thank you.
Oh, yeah. Yeah, I think until you find out the best practices in your area. I would link it but not everybody does. So, you know, it’s important. Of course, I would link it but then I would have all the other documentation to go through and say oh, yeah, this is, you know, this is what the provider is stating. Let’s see. Kathleen says watching this I realize is systolic is left and Sinister equals left and diastolic equals, right dextrous, right? So, it’s easy to remember. Yeah. Yeah. That’s a good point. I like that very very good. Oh, right. Thanks. Anything that allows you to help remember is excellent on my part.
Documentation
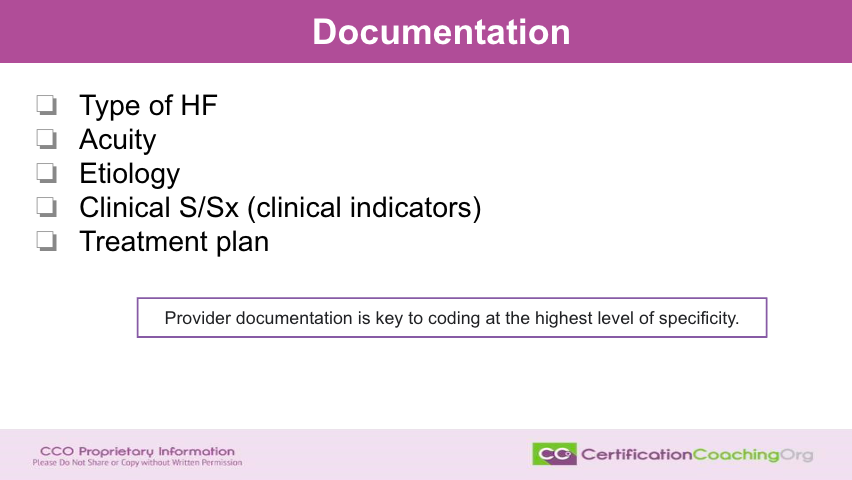
So, the documentation. What do we want to see in the documentation? Because the code set allows for the specificity, the first thing we want to know is what type of heart failure the patient has. We know that there’s more than one type. We just talked about two types, but there’s also chronic and acute, acute on chronic, right and we know the stages. The different stages signify the type. What’s the acuity of heart failure? What’s the etiology? What’s causing it? Is there something that has caused it? What are the clinical signs and symptoms or the indicators? And then, the treatment plan. All of this is really good documentation. Not only to allow us to get to the highest specificity for the code set but also for the provider to show the medical decision making.
So, as our E/M is based on medical decision making and time, if you have acute on chronic, you know, right-sided CHF that has, you know, an exacerbation and others not able to take a specific medication due to intolerance. Doesn’t that bump up the medical decision making and you’ve shown that all in the documentation? The provider’s documentation is always going to be key for us to be able to determine. What is the proper code to translate? Why? Because we code for statistical purposes. It happens to be a convenient way to get paid. I say that all the time and it is so true.
Example 1
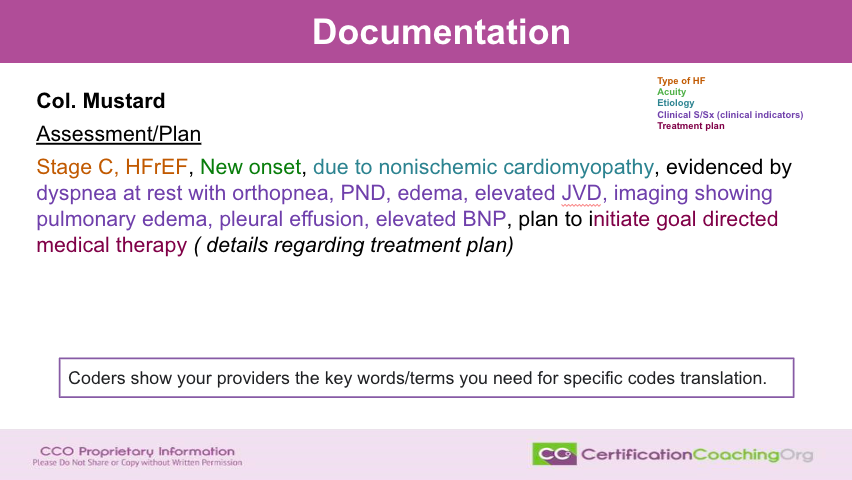
Let’s look at some examples now. This is the fun part guys. Let’s talk about and I put a little cheat sheet off to the side where I color coded these for us. First in orange, we’re going to signify in the documentation the type of heart failure. When it’s green, that’s going to give us acuity. When it’s that teal color, it’s the etiology. The clinical signs and symptoms are going to be purple and then that’s kind of a burgundy color is going to give us the treatment plan.
Now, real quick before we break this down. Notice in the box below. The coders show your providers the keywords and terms. You need to specify code translations. We’re translating for the providers. We need to let them know. Hey, if we have this documentation or give them even examples that you don’t have to make it as wordy as this. Some of this is evidence that could be in the exam part. It doesn’t have to all be in the assessment and plan. But, if you have an assessment of a plan that’s like this, brilliant. We’re able to code to the highest specificity and it also shows the medical decision making that you’re doing.
Realena says I can see why coding of the medications can also help see the progression of, the progression or not towards heart failure. Yeah. Yeah, you’re right. The medications. I’ve also seen where it’ll say the allergies or the patients medications. They can’t tolerate and when you start seeing different types of blood pressure medications and medications commonly used for that the patient cannot take and I’ve even seen brilliant documentation where the provider goes ahead and links down there that says, you know, in the treatment plan that the patient because the patient is not able to take, you know, and they start listing off like two or three different medications. We’re now going to try, you know, a, b or c. Brilliant. Shows medical decision making. Let us also understand the progression of the disease process and allow us to know what to look for.
It gives us a heads up. Hey this may be changing. This is progressing. This code is probably going to change in the future. Good point. Now, let’s break this down. The type of this particular person has stage C and they put the HFrEF. If you get an ejection fraction study, now, we cannot take the diagnosis of systolic or diastolic from those studies. We’re not allowed to do that. That’s not our job. However, if the provider pulls the study into the document for that office visit for example, then we are. We’re able to say oh, they’re an HFrEF. That specificity the doctor picked in the EMR system I50.9 which means unspecified but they also have in the documentation that, you know, they’re left or the right then we can upgrade and use that because it’s in the document that the provider signed off on. Okay.
Now, the reason why it’s important for us to understand those codes as well as know. Moving forward. What is the specificity that’s available? So now, we have a new onset due to non-ischemic cardiomyopathy evidenced by dyspnea at rest with orthopnea. There’s a P&D. There’s edema elevated JVD. Imaging showing pulmonary edema. Pleural effusion. Elevated BNP. That is all signs and symptoms and plan to initiate goal directed medical therapy or details regarding whatever treatment plan the provider has chosen. That is what we’re looking for. That’s Colonel Mustard. I like to use the characters in games like clues for my patients. Did you notice that? Oh, right.
Example 2
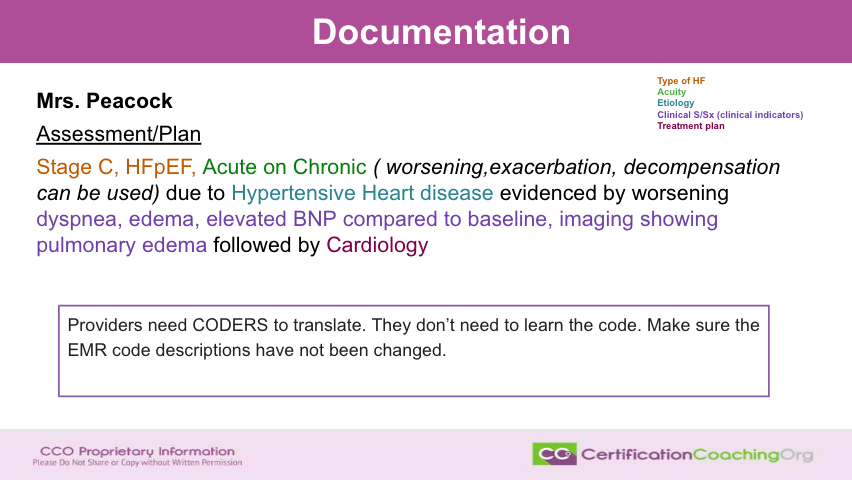
Okay, Mrs. Peacock. What about her? Well, stage C again. This time there’s a HFpEF, acute on chronic. Now other verbiage that could be used is worsening, exacerbated, decompensated, decompensation due to hypertensive heart disease evidence by worsening of dyspnea, edema, elevated BNP compared to baseline, imaging showing pulmonary edema. And what’s the treatment plan? Followed by Cardiology. Do we have to use it? Does a provider have to use all of that documentation? No, it could be just one word. Again, maybe worsening edema. That’s all you know, if that’s applicable for their patient but this is an example of the possibilities that are there.
Now note in the purple box here, providers need coders to translate. So as long as that information’s there, we can translate it to the highest specificity. They don’t have to learn the code. They don’t need to know that, you know, the difference between an I50.9 and I503.32. That’s not their concern. They need to know this is what I need to have in the assessment and plan for the coder to pick up the highest specificity. But one of the things that I’ve noticed that happens in a lot of EMR systems is at one time or another that somebody has gone in and changed the definitions in the code and that’s a problem.
So, an example of that is a patient that has say they are an HFpEF and when they type in I50.9, it comes up that they are chronic CHF, you know right-sided. No, that’s not what I50.9 translates to. It translates as congestive heart failure, unspecified or CHF unspecified. Not the same thing and therefore as we go in and we look at the EMR systems, we need to make sure we’re not just grabbing the codes that come up in the assessment plan because so many of them now show the code but it also gives the description and they’re not the same. We know what the translation actually is, right?
Example 3
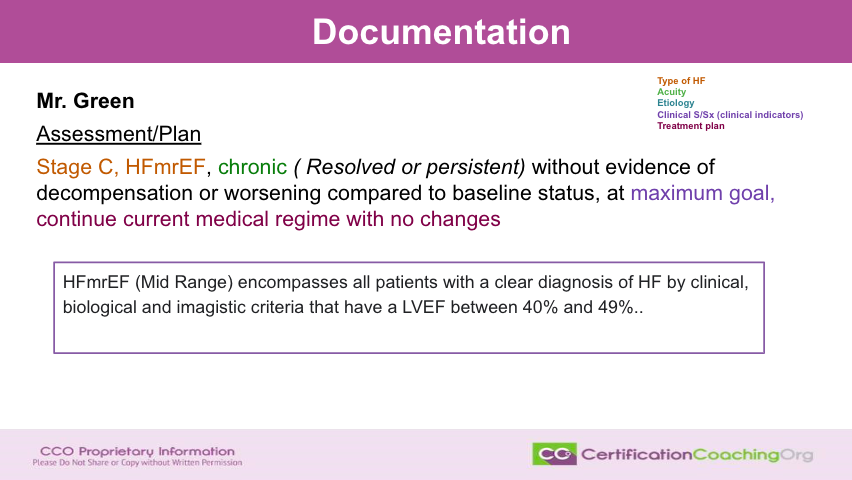
All right. What about Mr. Green? His assessment plan. He’s also a stage C but he is an HFmrEF. What does that mean? I’m going to tell you in a minute. Chronic. It could be resolved or persistent. Now again in the italics in the parenthetical I put I just put options without evidence of decompensation or worsening compared to baseline status at maximum goal and the plan is to continue the current medical regime with no changes. And if you didn’t know, “mr” stands for mid-range and it encompasses all patients with a clear diagnosis of heart failure by clinical biological and imaging criteria, but they have an LVEF between 40 and 49 percent. So, you learn something, right?
ICD-10-CM
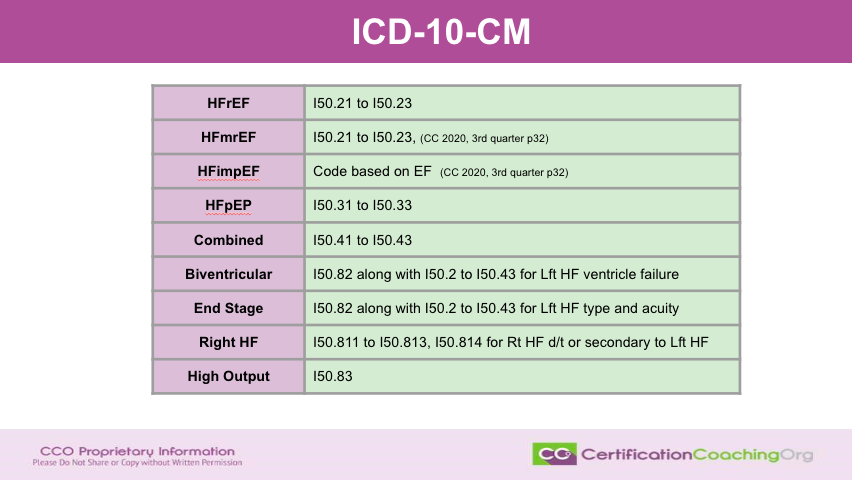
I got more information. This is the golden slide. This is the one that is going to break down and tell you about the codes that are going to help you translate. When you see the HFrEF, that means you’re going to be using I50.21 through I5 0.20. Now, if it is unspecified, you would use I50.20. But I didn’t put the unspecified in here. Then if they’re that “mr”, that is the same code because of the coding clinic and 2020 that came out third quarter page 32 that tells you that if it’s an HMrEF we’re going to use this code range. What if it’s an imp, improved MP? So, that would be the codes are based on the actual ejection fraction. That is also in the coding clinic. That same coding clinic. So, I would encourage you to go get that coding clinic. It’s quite extensive. Quite long or I would have been able to give it to you here. But now that you have that to reference.
Now, what about an HFpEF? That’s supposed to be EF not EP by the way, that would be an I50.31 through I50.33. But what if they have combined? There’s a code for that, I50.41 through I50.43. Now, we also have biventricular. Biventricular is going to be I50.82, but you’re going to also code the I502 code through the range I50.43 depending on which is relevant. So, this is for left heart failure or ventricular heart failure. If they are at in stage, this is I50.82 along with the applicable left heart failure type and acuity. For right heart failure, that is going to be I50.811 through I50.813. If the patient has right heart failure due to a secondary case of left heart failure, that’s I50.814. If they have high output, then that is considered I50.83. This is a quick reference that you can use. You could also take this into your provider and let them know. Hey, these are how this translates for quick reference if, you know, and you’d be able to put that in the pocket. We’re going to have this up as a freebie at the CCO website that I think will be beneficial to you as well.
Resources
Well, lots of resources that I used for this education and you’ll be able to tap into those, but absolutely know that we think that this career path is fun. That we enjoy what we do and we want you to also enjoy it. We want to be here as a resource to you. It’s always fun working with CCO. So, go to CCO.us.
Let us know what your thoughts are and what topics you need us to do.
More education on and then we’ll uh, so round back at the CCO club that you can find on cco.us where we can have more conversations about coding, the coding industry, billing and things like pharmacology, the disease process, pathophysiology, and what’s happening in the industry. All right guys. Thank you so much, and we’ll see you next time. Bye.
![[CCO] Certification Coaching Organization LLC [CCO] Certification Coaching Organization LLC](https://www.cco.us/wp-content/uploads/2015/05/CCO-Logo-2015-d3-500px.png)
If attending doctor documents Systolic but Cardiology documents Systolic and Diastolic – is Cardio being more specific or is this considered contradicting to what attending has documented?
Great question! It’s definitely not a contradiction, but more like different “zooms” on the same information.
The attending doctor gives a general overview with the systolic pressure, like a wide-angle lens. The cardiologist goes deeper with both systolic and diastolic, like a zoom-in for focused detail.
Both are valuable! The attending establishes the overall picture, while the cardiologist provides specialized insights. 🩺
Keep in mind:
Context matters: Consider why each doctor documented what they did.
Coding might require both values, even if only one was initially documented.
If anything seems off, clarify with both specialists for smooth sailing! ⛵️