CCO student asks, “Is it acceptable to code a working ICD diagnosis?” The student asked this question based on the textbook that she’s working on. “For the ICD code, do you code the symptoms or the working diagnosis?” This is a common question by new ICD-10 students and students in our ICD-10-CM Review Blitz.
Outpatient vs Inpatient Diagnoses
Physician and outpatient coders do not code working diagnoses, only definitive ones. So if there is no definitive diagnosis, we code the signs and symptoms. It’s totally legal to do that as they’re being worked up. For inpatients, they are able to code the working diagnosis. So that’s very good thinking.
And how do we know this? Just because we say so? No. We’ve got our ICD Guidelines and we recommend becoming familiar with them. Here is a screenshot from the current ICD-10-CM Guidelines about this topic in Section 3:
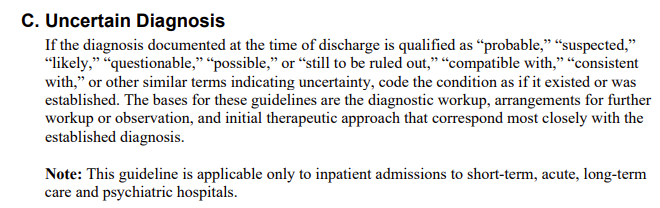
FY 2022 (October 1, 2021 – September 30, 2022)
Section III. Reporting Additional Diagnoses
It’s so important, they mentioned it several times. Uncertain Diagnoses is also covered in Section 2 as well as Section 4. So it all reads like that consistently.
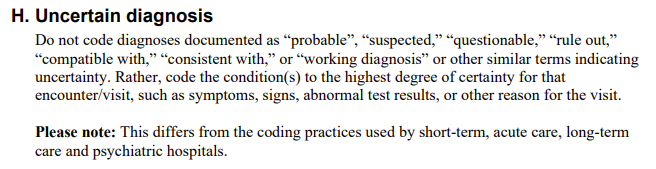
FY 2022 (October 1, 2021 – September 30, 2022)
Section IV.Diagnostic Coding and Reporting Guidelines for Outpatient Services
Age and certain diagnoses. If the diagnosis is documented at the time of discharge, it’s qualified as probable, suspected, likely, questionable, possible. We call it equivocal language: could be, maybe, kind of, sort of. Code the condition as if it existed or was established. This is what they’re telling inpatient coders to do.
First listed diagnosis vs Principal Diagnoses
This is for outpatient services. In the outpatient setting, the term ‘first listed diagnosis’ is used in lieu of principal diagnosis. Diagnoses often are not established at the time of the initial encounter. It may take 2 or more visits before the diagnosis is confirmed. The most critical rule involves beginning the search for correct code assignment to the alpha index.
Codes that describe symptoms and signs as opposed to diagnosis are acceptable for reporting purposes when a related definitive diagnosis has not been established or confirmed. So working diagnoses can be confirmed later on. But if it’s still a working diagnosis, it’s not confirmed yet so we don’t code it until it’s confirmed.
I always tell my students, “You don’t want to give them diabetes before they actually are diagnosed with diabetes.”
And that’s a very good point. I used to or I still do but when I first had migraines, they thought it was MS. And so all of my forms exclude MS. Well, along the way, they actually put in my chart like I had it which I didn’t. I came to find out it was a complicated migraine. So when I went to get insurance, life insurance, disability insurance, anything like that, they were denying me. And this was when I was a lot younger than I was and came to find out that was why. And it took a lot of work to get that off and then to realize, no that was not a working diagnosis. It was a rule-out diagnosis.
Working and rule out, they’re similar but it’s kind of like the opposite. The doctor, when they say rule out, it’s this thing that could be but probably not. They just want to rule it out and get it off the table. Where working ICD diagnosis is basically the physician knows what it is and is just trying to get confirmation.
![[CCO] Certification Coaching Organization LLC [CCO] Certification Coaching Organization LLC](https://www.cco.us/wp-content/uploads/2015/05/CCO-Logo-2015-d3-500px.png)