- Introduction
- Process of Elimination ICD-10
- 1st Character
- Causal Relationships
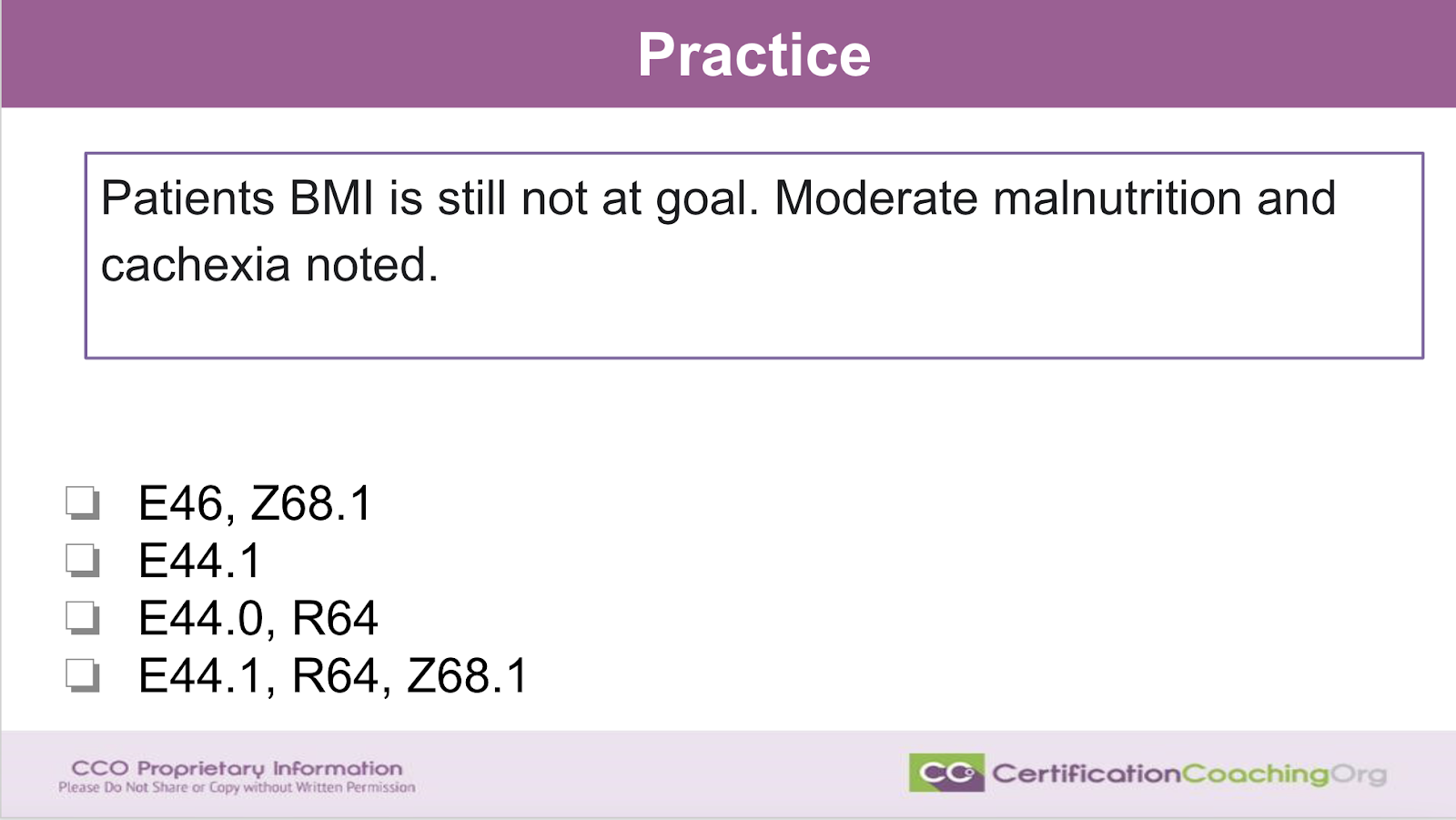
- Practice 1
- Practice 2
- Practice 3
Transcription Introduction
Hello everyone! Hey, it’s great to see you guys. Let’s see. Where’s everybody coming in from? Hey, you guys are already talking about our subject tonight. Thank you. You’re right. Sarah said I’m sure this is gonna be great because they know I love ICD-10. Obviously, Sarah has watched me present ICD-10 for a while. It’s kind of obvious how excited I get and Kimberly. Yep. You’re excited to hear what I say. Well, we’re gonna have fun tonight. I was just telling Jesus a moment ago that he always says, you know, have fun and off I go, oh I will tonight because it’s a subject I enjoyed.
Process of Elimination ICD-10
We are going to talk about the process of elimination and ICD-10. Now, this is going to work both if you’re getting ready to test and across the board. Any credential that uses ICD-10, you’re going to be able to use a few little tips that I’m going to give you but just in your daily work too as a coder. This is stuff that as you get under your belt, makes you faster and more accurate And don’t think that you ever get away from looking up codes. Sometimes, I amaze myself and I think I remember that code. Yeah. Yeah, you know and especially chronic conditions because I deal with them a lot. But if you start asking me things like what is you know bilateral titus media? I can’t tell you that. Now I could you know, I could tell you it’s an H code, but I can’t tell you what that is because I don’t work in Pediatrics. Most of my dealings every day are chronic conditions with risk adjustment. So and of course HHS for suggests, but predominantly I do CMS. So anything that happens to you when you get old on there.
Is this reviewed in depth with the CRC course? Sarah, we do deal a lot of this in the CRC course because well first of all because that’s part of my background. So anything that I can steer to educate in that venue, I will. Exactly, this will happen a lot with the CRC because these are chronic condition usually that you deal with all the time but this isn’t just for risk adjustment. We’re talking about all of the chronic, not all the chronic, all of the diagnoses that you could be tested on. We’re gonna again give you a few little ideas on ways to narrow down with the process of elimination and just some tips.
This is a CCO live event. So you’re always going to be able to come back and reference this in YouTube and more casual, right? So feel free to make comments. I’ll keep this eye looking at the this other screen, my other monitor and try to address any questions that you have along the way. Let’s get started. Process of elimination for ICD-10.
1st Character
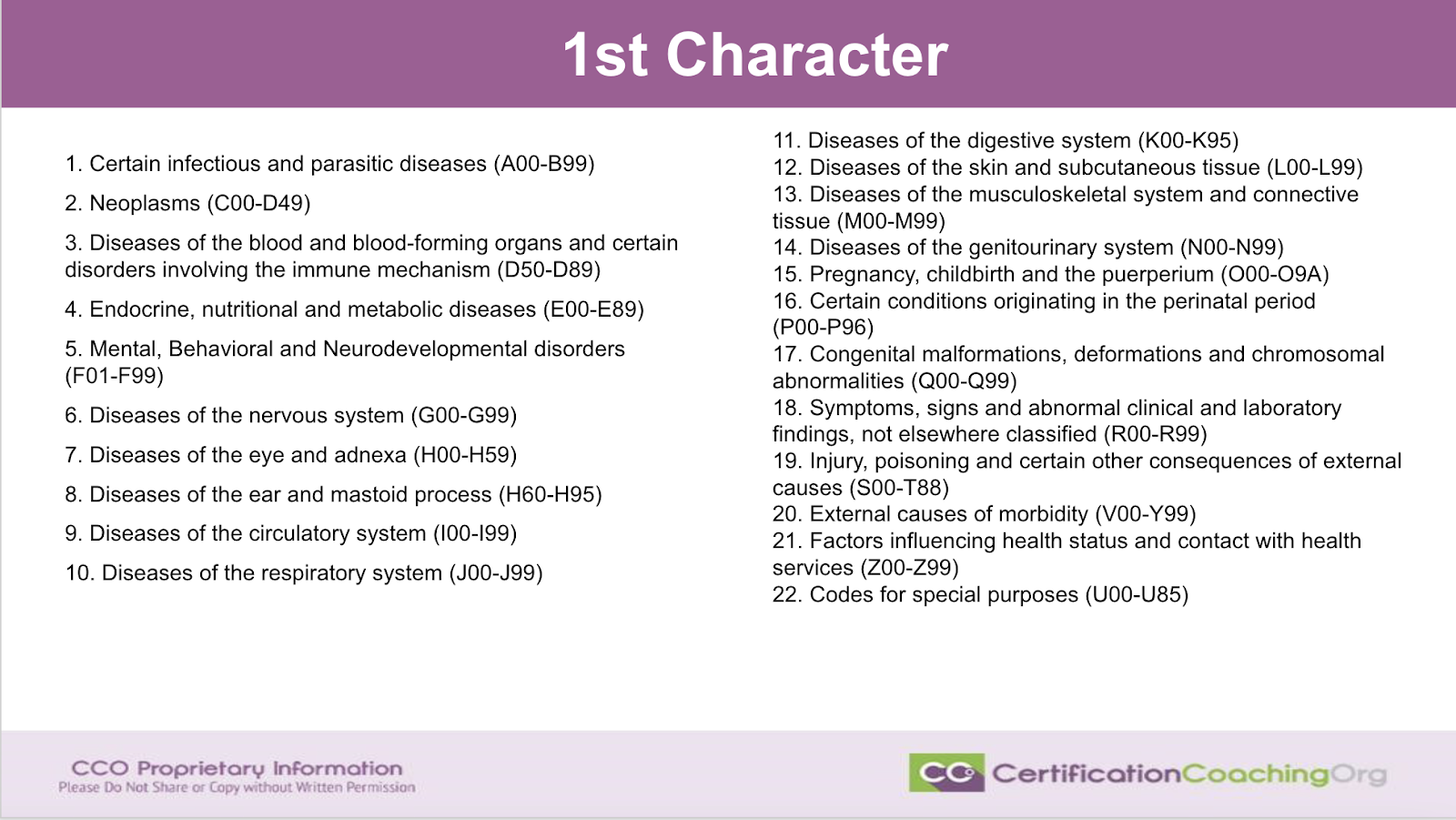
The first thing that you need to know and I apologize for this being a little bit smaller. However, I wanted to get everything on one screen. The first step when dealing with ICD-10 is to know the first character. So, if you don’t get anything else out of tonight, you need to memorize the first character. Now, I don’t mean memorize every single code. However, it follows the alphabet guys. You know the alphabet so you’re not going to have any trouble memorizing these. I’ve done this before with other videos. Let’s just real quickly highlight how to do this. If a code in ICD-10 starts with an A or B, then don’t think of certain infectious and parasitic diseases. That’s too much. You don’t have to memorize this. Note that it’s going to be some type of a bug. A bug. A, b. That’s how I remember it. It’s either going to be a parasite. That’s a bug. And again, it’s gonna be something in there that isn’t supposed to be there. A virus and an infection. Those are A and B codes.
So you don’t have to use my suggestion to get through these you can come up with whatever works and resonates with your little gray cells. Neoplasms. They’re all seeing decodes. Now, there are some other decodes that are diseases of the blood but for the most part, think C and D have to do with cancers and another little tap because it’s alphanumeric, think of how the neoplasm table is set up. It is set up to go through the body system. However, It is set up with the table so primary malignancy is first then secondary right and then it goes. Let’s see primary secondary, but not or cancer inside to benign, uncertain all this other stuff. I can’t remember the last three. But anyway, if it is a low number like C0 something, that’s primary cancer. By the time you get to D49, those are unspecified type cancers or benign cancers.
Okay, so it’s alphabetic numeric in that way. So if you have a choice and you see two codes that are cancer codes and you have one cancer, you can almost weed them out very quickly by looking at the numeric aspect of it. If it starts with a C and the number is higher then it’s probably secondary cancer or as cancer in situ versus a lower number will be the code for primary cancer. Now, do not do this for testing to her purposes. Always look up the code. But if you need to look at the options and we’ve got some examples here to kind of decide hmm, you know, is this going to be a, this is a secondary cancer and I’ve only you know, and I’ve this was a real hard question. I saved it to the last I’m gonna go back. I got to pick something. If it’s a secondary PEC cancer, and there’s two codes pick the higher number. I mean that’s gonna probably be right.
Diseases of the blood and those are going to be later D codes. Now, it only goes to D89. So anything from D50, remember? That’s another thing. D halfway to a hundred from D50 all the way out to the rest of the decodes are going to be blood codes. Polycytopenio, thrombocytopenia and things like that. E, endocrine codes. Predominantly, you’re going to be tested on things regarding diabetes. But anything that has to do with the endocrine system starts with an E. When you look at F codes, they’re codes that make you feel funny kind of, you know, funny for me type thing. Nervous system is G Codes. There’s two things. You can remember either Hercules Perot from Agatha Christie, they always said little gray cells and that’s actually what you call them. They’re gray cells in your brain or ganglia part of your brain. Then H codes are eyes and ears, hearing then let’s see then you get into circulatory system. Anything to have with ischemia or the heart think I heart, right?
J codes. I was telling everybody about breathing the little when you work on an ambulance. If you need to make sure the airways patented person’s unconscious. They have this little device that looks like a j and you stick it in their mouth and you turn it sideways. You measure it from the corner of their mouth to their ear. I always remember that but one person told me a student one time told me what looks like a fish hook and a fish can’t breathe out of water. So, they’re breathing, right? That was really good. K codes – digestive system. Special case, serial. L everything to do with the skin. If you want your skin to be luscious, then you’re going to use an L code. M code – muscular skeletal system. M’s in anything with a genitourinary system. Gosh, how do we remember? No, you have to go to the bathroom. No, let’s see. O for obstetrics. P for Pediatrics. Q if you were born a little quirky because they’re congenital codes.
R codes are signs and symptoms. S codes will be where you they’ll be like broken bone codes. S and T’s – injuries and stuff. External causes of morbidity – V and Y. Z codes, everything elsE. Wverything that tells the rest of the story. These are history of codes, status codes. I got ran over by a tractor in a parade codes. Just weird things and then of course they added those U codes for codes for special purposes. If they give you U code, it’s probably covid. At least, that’s what they’re testing you on. Sarah says I hope you come up with these analogies for ICD 11. Of course, I will because this is the only way I can make my head memorize it and they are not that hard. It will not be the same. So, you’re gonna memorize this and then when we switch over to 11, we’re gonna learn a new code set, but it’s predominantly the same thing. Get in there and start practicing with it. I have already started working with ICD 11. It’s going to be fun, but don’t get me off on a tangent.
Causal Relationships
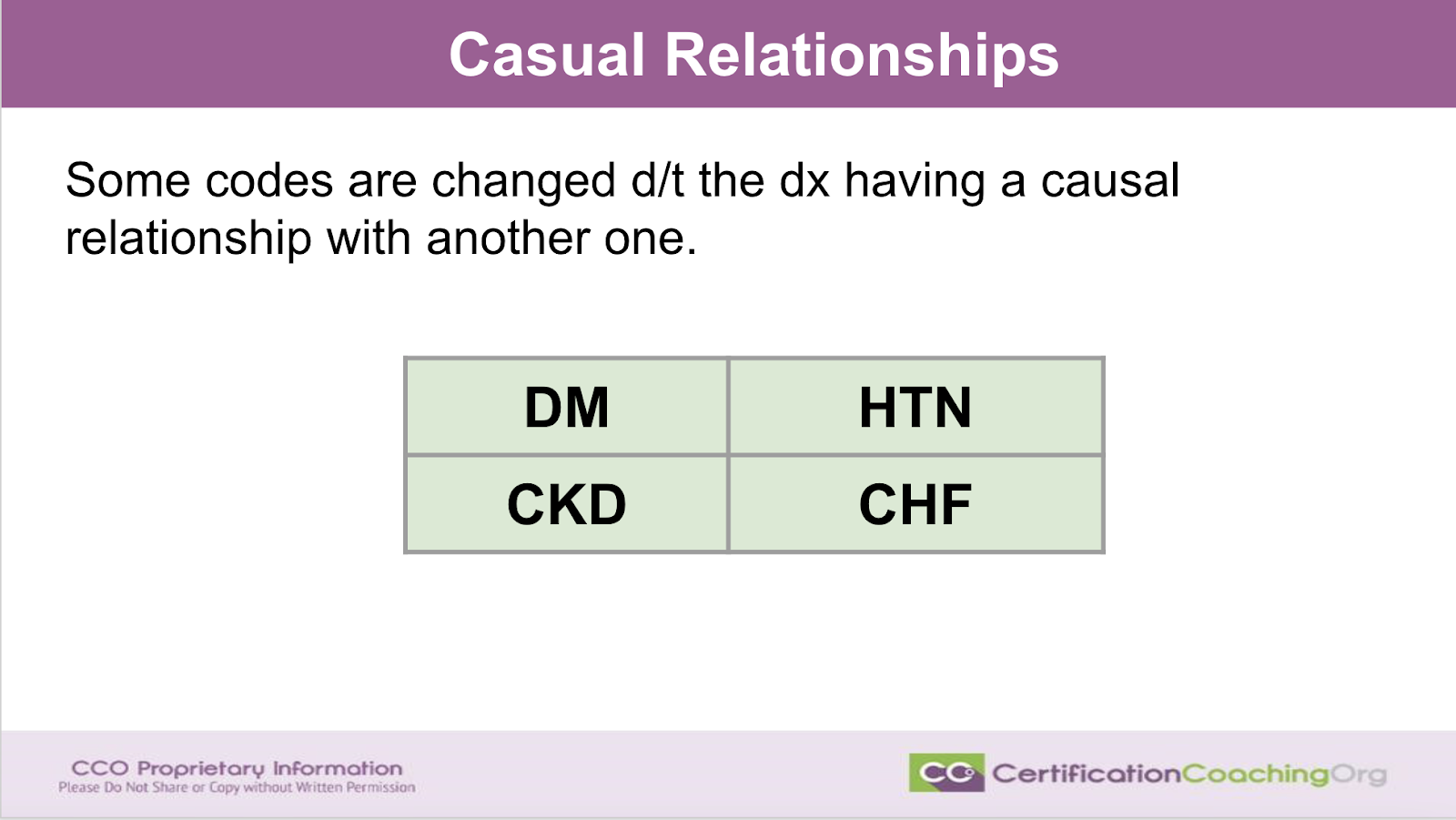
Now the next thing you need to remember when dealing with ICD and ruling out process of the elimination is you have to remember that it follows the disease process. Now what is my mantra that I tell everybody all the time? Why do we code?I bet you guys could probably type it out in the chat. How many of you guys remember what I say all the time? I’ll give you a few minutes to type it out while I tell you why it’s important to know causal relationships. It’s built into the code set and some codes are going to change due to the diagnosis having a causal relationship with another one. These are the heavy hitters diabetes, hypertension, CKD and CHF. Now, there are other ones but these are the ones that you’re going to be tested on and that you’re going to see daily that have combo codes and causal relationships that’s going to change the code. Yes. That’s right. Statistical purpose happens to be a great way of reimbursement. You’re right. That’s not exactly the way I say it but that is the gist. We code for statistical purposes. It happens to be a convenient way to get paid.
So therefore, we’re translating the documentation of the provider into another language, a code set so that we can capture its capture the statistics. That’s why there’s causal relationships built into the code set. The disease process, it’s necessary for the disease process to be described. And again, if a patient has diabetes and they have a comorbidity within the diabetes, we know because of statistics. What organ systems are mostly affected by diabetes? And it’s going to be the kidneys the eyes. I’m going down because kidneys is a two. It’s you know, like E112. The eyes is 3. 4 is neurological. 5 is the heart. 6 is the skin and everything else and nine is no comorbidities. That’s another thing you should memorize guys and we’ve done that on another presentation just recently.
So, go in and write E11.2, renal kidneys because you got two kidneys. E11.33, you got two eyes and if you’re a parent you have an eye in the back of your head or think, you know, people have a third eye. 3 is always eye complications. 4, you got four extremities. Neurological is 4 and it usually is. Things like poly neuropathy for extremities is neuro. 5 is going to be the heart. Now, how did someone say that the other day and I thought oh, you’re so smart. I had not thought about that in 5. Now, I can’t remember what it was. And then 6 is skin and everything else, right? So, make yourself a note for that so that you’ll be able to look at diabetic codes really quickly. Hypertension and CKD changes the hypertension code. We have different codes for hypertension. We have I10. Remember I10 is the first code most people learn and it’s kind of a no-brainer. We work in ICD-10 hypertension. Everybody has it. I10 but if the person has hypertensive heart disease, that’s I11 not I10. And if a person has a kidney complication to diseases, it’s a I12 because the hearts involved and the kidneys are involved, too.
If you have three things going on 3 disease processes, you have hypertensive heart, you have CKD and you got CHF heart failure, I13. Hah, see how easy that is now. Oh, hand over your heart. Five fingers on Natasha. You remembered. It may have been you that said that. That’s right. I knew there was a great way. You put your five fingers over your heart and that’s how you can remember that five is the heart. You guys are savvy. Again, study up on these codes. The codes surrounding diabetes, hypertension, CKD and, CHF because they do change with the disease process. CKD, pretty darn easy because the stage follows the last character. If you’re a stage one, .1 in 18.1, if your stage two, .2. Three, .3, .4, .5, .6. It doesn’t go up past six. Well, it had unspecified would be a 9 and then CHF.
I50.9 means you have CHF but you don’t have any other information and there’s a place for that because if you were newly diagnosed with CHF, they need to send you off to the cardiologist or get in, you know, ejection fraction study. They need to do an echo. They got to do other things just find out what type of CHF you have and the type is determined on what side of the heart is being affected. Is it the left side or the right side of the heart? That will tell you if you have systolic or diastolic. If it’s both sides of the heart, it’s a diastolic and systolic or systolic on diastolic. It doesn’t really matter. It’s because you got both of them. Okay?
Now that is a really interesting side rail that I won’t get on but I did get to listen to a fabulous cardiologist in Fort Worth the other day at one of the local chapter conferences and I reached out to him and we’re going to get him as a guest speaker because he had some great analogies and things to tell you about especially CHF and I was writing notes just as fast as I could and then I thought I will just get him to speak for us and then we’ll have it on the record. It was really really good and very very funny.
Practice 1
All right, let’s talk about practice. Let’s put these few things that I’ve already told you into practice and I’m going to give you some suggestions. But what I want you to do is use this thought process. However, it’s going to resonate with you and then you’re going to use it for yourself. So you’re gonna look. You’re gonna understand how to translate this language. There’s one thing that you do. You learn how to look at the code and translate. Okay? That’s what happens in the beginning and that would be as if you know, you took four years of high school Spanish and you know, you could read a book in Spanish. You can even write a letter in Spanish and stuff, but you’re really not fluent but you you could get by very very well, right? All right, but after you get a little time under your belt and you really study the code set and the stuff falls into place. That’s when you get fluent. Oh my gosh, I like the way that sounded. I am going to tell people from now on I am fluent and ICD-10 because I think in ICD-10 now, it’s just such a fun code set.
All right. Let’s do our first practice. Patient’s BMI is still not at goal. Moderate malnutrition and cachexia noted. With that being said nobody’s looking up any codes at this point. What do you see in front of you? You see four choices. Now if you know that the patient has malnutrition then are you thinking that’s an E code or would that be an R code, right? R codes, what did I say? They are signs and symptom codes. But malnutrition, that’s actually a definitive diagnosis. So, just out of curiosity. Let’s say this is A, B, C and D if you don’t be looking these up.
If you just had a gut feeling on what you see here, which one of these would you suspect is the correct answer A, B, C or D? Maybe I should have used A, B, C or D but I just did the bullets instead. I’m really curious what your thought process is and then I’m going to tell you how my brain works if I didn’t have these codes memorized, but I just happened to have a memorized so kudos to me. Okay, C. Lots of people saying C. Very good, Okay. Hmm. Now if you’re going to break down the process of elimination, the first thing we have to do, Kimberly says D, is know a few things about the code.
Who knows what BMI codes are? They’re Z codes. Oh, we got an A in there. I’m enjoying that you guys are getting really, I’m really glad because you guys are going with your gut. Okay, we have everything covered. Nobody said B. That’s okay because they know that it’s more than one code. Right? Right. So again, this statement tells us there’s probably more than one code because the person has moderate malnutrition and cachexia. How many you even know what cachexia is? Do you even know is cachexia a sign or symptom of malnutrition? If it is then it wouldn’t get coded. Maybe. Okay. What if I tell you yeah, okay. What if I told you that? Okay. The BMIs are Z codes? There’s Z68 codes. And just a little sideline, if you have a BMI of 40 and above that would be morbid obesity and that risk adjusts.
But we’re not doing risk adjustment. We just need to code out what stated here and the first thing that you know if you knew that a BMI code was a Z68 code you would probably latch on to that right away and think okay. Well it states the patient has a BMI. So, it’s got to be A or C or D. But the problem here guys is what is the BMI? BMI is not a diagnosis. BMI as something that you have. So. Z68.1 is a BMI of 19 and there’s a code range there but it’s around 19. But you have to have a BMI stated the number to be able to code it. And since we don’t have a number, we cannot code Z68.1 because there’s no BMI listed. Therefore, A and D are knocked out.
Now if they said the patient’s BMI was 19 and not a goal, you’ve got a BMI the number because that character after the decimal indicates what the BMI is. Now, it’s not one, two, three. It’s a weird number but I’m telling you that we don’t have a BMI. We just know the patient’s BMI was not at goal. So, A and D is automatically out. We don’t have that information. Okay, malnutrition and cachexia. You don’t know what cachexia is so you gotta wait on that and you have malnutrition. Another tip, when you see descriptive verbiage like mild, moderate and severe, I guarantee you it’s going to be a level in a code, right? Morbid obesity, severe obesity. Just obesity by itself, you know, that’s two different different codes. So, you’ll have mild, moderate, and severe a lot in descriptive words in the code set and that changes the code.
That being said, E46 is going to be, you know, you think okay. Well our E code is our malnutrition but we have moderate malnutrition. A giveaway is if you don’t have a decimal then you can’t describe mild, moderate, severe because it’s not. All those descriptive terms are after the decimal usually like 98.72% of the time in the code set. So, the fact that E46 doesn’t have descriptions, you know, anything after the decimal I would have tossed that out in my brain If I was quickly thinking. Actually, E46 is the code for, it is a malnutrition unspecified. I believe. I can’t remember exactly it’s something like that. So, I know my code is probably going to be 0.1 or .0 and E44 is gonna be malnutrition. So, I already ruled out A though because Z68.1, I can’t use that. So, that whole thing is out. So I know E44 is going to be malnutrition. I still haven’t looked up a code.
So is it zero or is it a one? Now, are we gonna do just one code? Hmm. Whenever you see moderate or whenever you see a diagnosis that you don’t know is a sign or symptom, that tells you that you don’t understand the disease process enough and that’s not a good thing. Cachexia is something that a person gets when their body is wasting away. It actually is like the body starts eating the muscle and they’ll get this concave look by their eyes, the sunken cheeks. They can see it in the armpit and different places. It is a wasting part of but it’s more than that because a person that is obese can still have malnutrition. A person that is obese, can a person that’s obese have cachexia? I know they can have my nutrition. I don’t know if they have cachexia or not. Anyway, it’s a wasting away. Let’s see.
Jane says, okay, a question. Doc documents assessment BMI elevated. I think doc says that something that when not want to say obesity. I do not look for BMI if on record, yeah, well, that’s just wrong. Don’t give me on that tangent Jane. The the reason they don’t want to say obesity is because they have to give the patient that document. Their assessment when they walk out and they get upset. No. Nobody wants to be called obese. Let alone morbidly obese. However, you could put the BMI on there but if they don’t diagnose morbid obesity or obesity, it doesn’t get captured for the RAS score nor does it captured for the statistics. So again, we don’t want to do just BMI alone. So, code without decimal is the base coat and after decimal is a description. Makes complete sense. You’re right Kimberly. Now, that is not true 100% of the time.
Okay, but for the most part if you’re having to rule out and look at questions and processes of elimination, that’s going to do it. The last character is also going to be giveaways. And while I’m on that, I want you guys to write this down because I just thought of this and I did not put it in the slide deck. If it’s an 8, so anything .8 or 8 at the end of the code? that usually means other and other is defined by the code set is the provider defined it. There is a description there. However, there isn’t a code for it yet. So that’s what other is and then if it’s a 9 that usually means unspecified meaning tdhe doctor doesn’t know yet. They still have to do more testing. And then once the testing is done, then they can come back and define it. And if there is no code to define what they’ve stated it is then you would use an 8, right?
Now, again, this is not 100% of the time in the code set but I would say it’s, you know, more than 90% of the time. There are a lot of codes that don’t do that, but that is another tip that I should have put in this slide deck. I can’t believe I forgot to tell you that but I’m telling you now 8s and 9s define them. Those are quick giveaways. All right. If we don’t know if it’s a 0.1 or a .0 for the malnutrition the fact that it’s moderate, it ends up usually being mild, moderate and severe then we know that there’s going to be two codes because cachexia is not. It is another diagnosis and the fact that they say, you know, malnutrition and caheaxia that kind of helps you there. So, I would pick C in this and actually I would be right but you can’t use. You can’t think mild is a 01 is moderate and 2 is severe or however, you can’t. You can’t do that because sometimes it’s not it goes the other way and actually with malnutrition it does. The higher number ends up being mild and moderate and then severe is the lower number. This is really weird but it goes backwards. Usually, it doesn’t do that.
All right. So, now we know without having looked up a single code which one we would go with if we were in a hurry or if we wanted to weed out. So what are we going to do when we do kind of narrow this down really quickly? We know that the first thing I need to know look up is E44.01. It’s not going to take very long and you know that cachexia is an R code because cachexia is a sign in symptom but it does have its own. It isn’t one of those things that you don’t code if it’s a sign symptom of malnutrition. It does get coded. All right. Let’s move to the next one. I think I’ve worked that one to death.
Practice 2
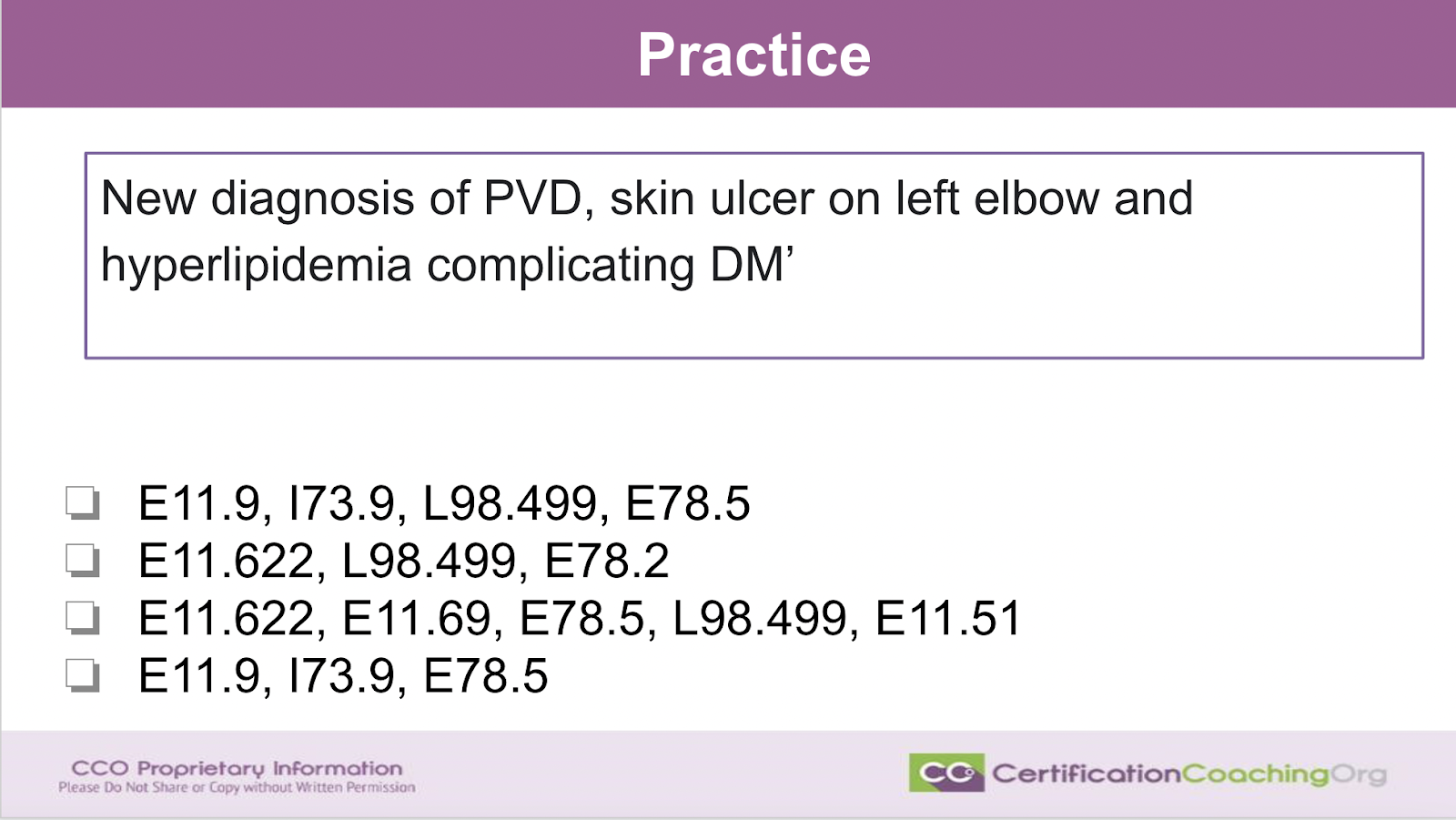
Here is a fun one. This is one that I give advanced students to see if they’ve got it. If they can figure it out. So, we have a new diagnosis of PVD. Skin ulcer on left elbow and hyperlipidemia complicating diabetes. What is the first code that you’re going to look at to rule out? I’m really curious what you guys think. Just give this the old Harry coating eyeball or what are your little coding Spidey senses telling you? If you had to pick A, B, C or D which one leaps out at you? First and I’m just going to take a little sip of drink of my mango juice while you know, I’m gonna keep my eye on there. Come on guys. Look at that really quickly. Don’t overthink it. Don’t be looking up codes. Just guess which one would you think it is quickly?
Because if you wait too long that tells me you’re looking it up. Okay. C to remove. Okay. The first of the last is the one. Now wait, which okay, you’re saying that the answer most everybody’s going with c.
Jane are you saying the first or the last that you think it’s the first or the last one? Okay. You see there is no D, Lisa. Oh, no, I’m sorry E. I looked at that wrong. It’s getting late in the day A,B,C,D. Sorry Lisa, okay. All right. Very good. You guys did a good job. All right, the first thing that’s gonna allow you to rule out any one of these is whenever a person has any type of skin condition, ulcer or whatever, you always have to stage it. No matter what all ulcers have to be staged. So, what are skin codes? L. We want luscious, longevity in our skin. No wrinkles. L codes. So, this has to have an L code. Whichever one is of those does not have an L code listed gets tossed. That’s D. D is tossed. There is no L code and we have an ulcer on the left elbow and it doesn’t matter if you got a combo code or anything. You have to have an L code. It’s a guideline. Excuse me to stage all ulcers.
So, we know that the last ones out. These out. Just draw a line through it. Next, how can you rule out another one of these? Right? We toss out D. The next one, we’re going to toss out is, Kimberly says toss out B. Why are we tossing out B Kimberly? I’m curious as to what you’re thinking is. Tell me why you toss out B. Because I was going to go with another code to rule out first. No, B is good Jane said, okay. All right. I would toss out A. Just got in. Going to listen only. Okay. Why are you tossing A? Mix hyperlipidemia. All right. The that’s a really good one. Okay. The next thing I would look at is your diabetic codes. E11.9 means the patient has no diabetic complications. Does this person have a diabetic complication? Is there any causal relationships within this description? There is. They’re all over the place. So, first of all, you have to know what PVD is. It’s peripheral vascular disease and whenever you have a diabetic with a skin condition, you got to code that. So, we’re going to be coding for, there’s complications here. Anytime a diabetic has an ulcer.
Boom, it’s not going to be an E11.9. So, any one of these choices that’s E11.9, toss. That’s a dead giveaway. They will do that in testing a lot. They will also put E11.9 with other diabetic codes. Toss it. Absolutely not you can’t do that. You can’t say oh my patient has no complications to their diabetes, but they have a skin ulcer and so now I’m going to code the diabetic with the skin ulcer code. No, you can’t do that. Okay. The diabetes and PVD, that’s right. There’s complication. There’s a code for that. So, now we’ve tossed A out and we’ve tossed D out. We’re left with B and C. Now, someone nailed the next code that I would have looked at to rule this out. Is that hyperlipidemia code? E78 is hyperlipidemia but after the decimal describes what type of hyperlipidemia and they said mixed hyperlipidemia. So, I just happened to know that mixed hyperlipidemia is E78.2. I think hyperlipidemia unspecified is 5. I think.
Let me just double check that. I don’t want to make a liar out of myself. I just happen to have the encoder open over here. Now that I’m getting tired, I don’t want to say that. Let’s see E78.2. Yes, mix hyperlipidemia is a 2. 5 is unspecified. Hold on. I’ll show you here real quick. Just bring it over. Look at there. Mixed hyperlipidemia is a 2 and hyperlipidemia unspecified is a five. You might want to memorize that because you see a whole lot of hyperlipidemia in your daily coding. All right. So, what type of hyperlipidemia does this patient have? We don’t know so it’s unspecified. So, it can’t be E78.2. That would be incorrect. So, we just ruled out A, B and D. Now, you may feel a little bit panicked. Will you have this available after the live lesson? Yes Maria. This is going to stay up on YouTube. So share with all your friends and Gloria makes another point. I73.9 gets tossed. You know why it gets cost because you’re the diabetic code takes care of it.
When a patient has diabetes and PVD, that angiopathy, then you would use the diabetic with angiopathy and it doesn’t tell you to also code PVD because you only code an additional code to further describe what the the diabetic complication is and that would be saying oh my patient has diabetic PVD or angiopathy. And by the way, they have PVD also. So my my patient has PVD complicating their diabetes. Oh and they have PVD also. No, you don’t do that. Now if your patient has CKD, oh, my patient is diabetic. They have CKD or if they have CKD I need to know what stage it is. Oh, okay, then I’ll do a CKD stage code. Same thing with the patient that has an ulcer and they’re a diabetic. My patient has a diabetic foot ulcer. Oh they do. Okay. Well, then you got to tell me where the ulcer is and what stage it is. Oh, okay. Well, that would be an L code.
See what I mean? So, very good. And let’s just real quickly, let me run through what these codes are. When you see E11.622, 6 is skin conditions and everything else. So, 622 is the diabetic skin ulcer. Then E11.69 is interesting because they stated hyperlipidemia complicating diabetes. That’s not a causal relationship. And so, it would be E11 type 2 diabetes with other complication. What’s the other complication? Hyperlipidemia, 9. E11.69 takes care of that. So, what is the other complication because other is something else? Oh, it’s hyperlipidemia but I don’t know what type. So, it’s E78.5. So, now you’ve described that. Oh, there’s your L code. I got it explain the stage of the ulcer and you look at that. You say well, what’s E11.51? That’s the PVD. Diabetic with PVD or angiopathy. All right, we did it. Okay. Let’s go to the next one. Wait, I got to use my my cursor.
Practice 3
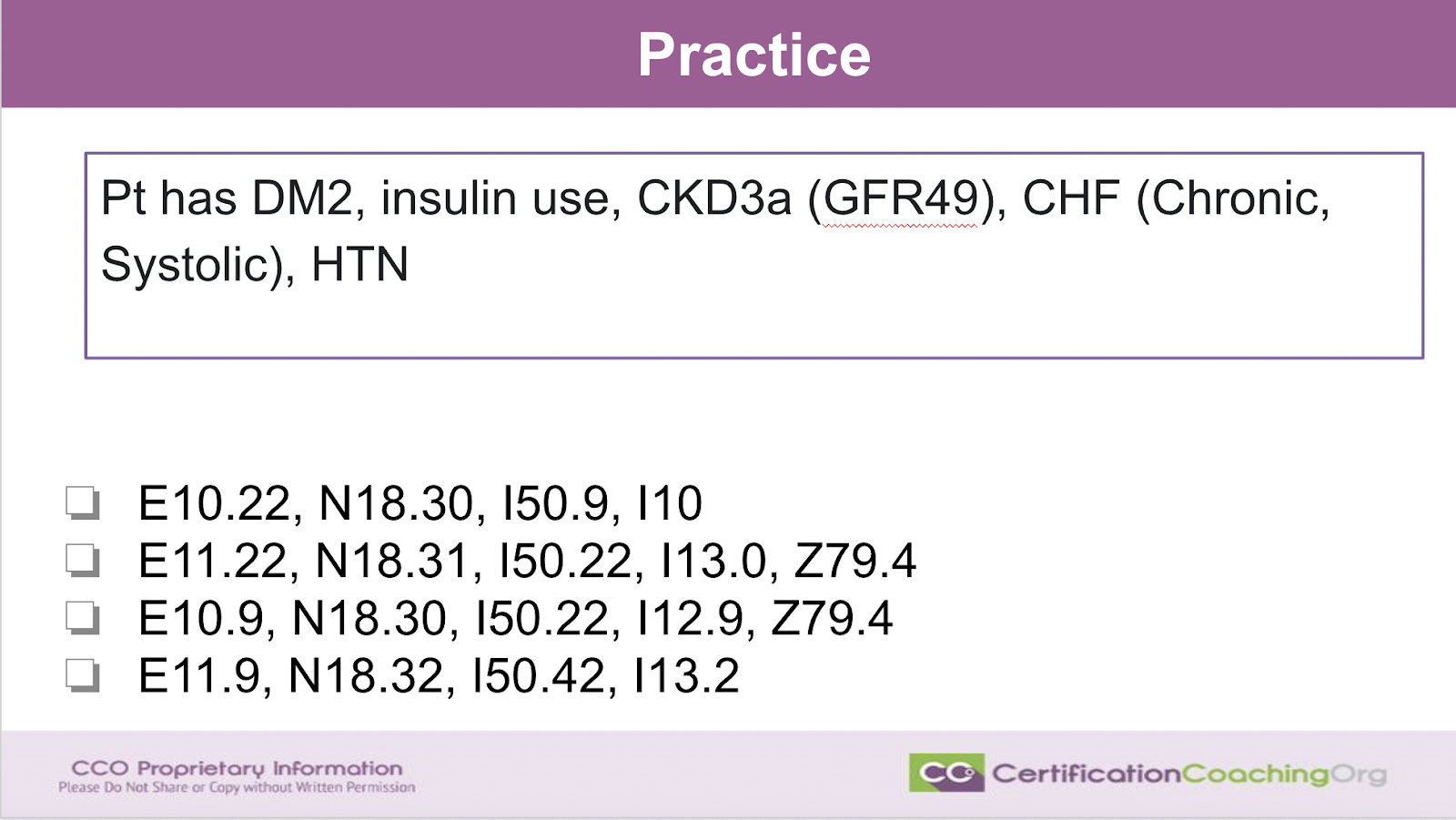
Alright. Now, we got a another one. Diabetic code. Give this one the old Spidey senses. What do you see guys? What do you see? What is the first code that you’re going to look at? That’s going to allow you to rule out? There’s a whole bunch that I could roll out just by eyeballing this. Anybody? Come on real quickly guys, tell me what you’re thinking. Don’t overthink. It don’t go look it up in the book. Just let your gut tell you what’s the first thing you’re going to look at. Stages of CKD. Excellent. You’re right. That’s very. Insulin use. Absolutely the I-10 code. Yes. You guys got it. Type 2 DM is E11. You’re right see? Okay. So let’s start at the end. I often look at the end of the list that they give you because this is really really common.
This would be a classic test question. In fact, they would probably word it up a little bit more but it’s not uncommon for them to give you five, six codes that you have to go through. Okay, and that’s gonna make you sweat a little bit when you open up that test booklet and you oh my gosh, you know the very first question. I got a little bit of all these codes. No, you don’t. You narrow it down. I have a patient that’s a diabetic. They’re type 2 and so they’re on insulin. I have to say they’re long-term insulin use. That’s Z79.4. You might as well just keep that under your belt. Memorize that. You’re going to see it a lot. So, since I know that’s a z code, there’s no other Z codes. You don’t even have to have it memorized Z79.4.
I know it’s a Z code and I have to have a Z code because it’s insulin use and so that means I can automatically knock out A and D because there’s only two choices that have type 2 or have insulin. So, now we know it’s B or C. See how quickly I knocked out those codes and we haven’t looked at any of them yet. Now the very next step. What do you thinking, right? We know it’s either B or C. We have a type 2 diabetic. What do we know about diabetic, diabetes? How do we code it? Yeah, that’s right Deborah. It’s B Because type 2 diabetes is E11. Type one diabetes is E10. So, we don’t have to look anything else up. We automatically know it has to be B.
We don’t have a choice because they’re on insulin and there are type 2 diabetic. Okay. Now, let’s break down why B is the correct answer? The first thing. We know it can’t be E11.9 because they have CKD and CHF and those are causal relationships. So it can’t be E11.9. They have complications but if a person has diabetes and CKD, that’s a two. They have two kidneys. So, it’ll be a .22. Now, it could be. There’s only like three diabetes codes for renal conditions and one is for diabetic retinopathy and the other ones for CKD and almost all the time they’ll test you on CKD and that’s a 22. So, think of this way. I got two kidneys, 1, 2 so I’m gonna listen to twice. Do you guys remember Sesame Street? So E11.22. Now, CKD3 used to be N18.30 but then they gave us more options. The A and B and since this is a it can’t not be 0.30 anymore.
So again, it’s got to be for A or B. It’s going to be a 1 or a 2 and it just so happens to be an A is a 1 and a 2 is a B. Then we look at our CHF code I50. Very common. If we didn’t know what type of CHF the patient had it would be I50.9 but we’re told it’s chronic systolic and just happens to be a two. So, it’s .22. Now, 0.42 is systolic on diastolic or diastolic on systolic. I just have known that’s both of them. Then our hypertension code. Because we have hypertension in CKD and CHF, it changes the hypertension code. So, I10 is out. We actually have three processes. We have CKD hypertension, CHF. So it’s a three. So, I10 and I12, out the door. If they just had CKD, two things. So, it would be I12 and then we have our insulin. That’s how my brain works, guys.
But we ruled it out on the last code and the first code and that was an intimidating at all. Was it? You were able to rule those out quickly immediately because you became fluent in the code set. Now, don’t expect this to happen right away. If you’re a student, this you know takes time. This reminds me of my mother teaching painting classes and they would sit down and she would paint these beautiful roses with like tole paint that you know, acrylic learning classes and the students will get so frustrated. I could hear them when I was growing up saying, how come I can’t make my flowers look like yours and she’s would say because you’ve painted five so far and I’ve painted over a hundred thousand. That could be it.
So, you know, I have a over a decade of working with the code sets and the way they work and some of you guys are just starting but it’ll come. The more you hear these little tips and tricks right and how you understand the disease process and you get to write all over your if you’re taking the AAPC manual test you get to write on your manual and make yourself a little notes. So, you can help yourself that way.
Now, if you have a topic that you would like us to do a webinar like this, break it out. Maybe discuss it or maybe you’re struggling as a student with a particular area then let us know and we’ll create some education surrounding it. It’s really easy to submit your request. It’s CCO.us/topic-request. If this was beneficial to you, you know, you guys, we don’t really advertise. So, as a thank you to us, might be kind of nice if you let other people know that we have this YouTube channel. We’re on Facebook. We are also on LinkedIn. You can share, you know, our site on LinkedIn. Again, but we have fun doing this. We want to give back but we don’t know what you need unless you tell us. So, give us a topic request and that’s it guys.
If you are learning and you want to have fun when you learn, reach out to us at CCO.us and kind of let our enjoyment of the code set rub off on you. Alright. Thanks, guys.
![[CCO] Certification Coaching Organization LLC [CCO] Certification Coaching Organization LLC](https://www.cco.us/wp-content/uploads/2015/05/CCO-Logo-2015-d3-500px.png)
