Hello everyone! How are you doing? I am so glad to be joining you today with the topic that I know will interest you. This is our Live with CCO. We’re in episode #86. The Live with CCOs are more casual. We have a lot. We answer questions along the way. So, feel free to make a comment in the chat. Let us know where you’re from. If you have any questions, I’ll keep an eye on the screen to answer those as we move forward. I wanted to let you know that we’re so close to our one hundredth. Can you believe that? One hundredth episode of our CCO Lives or Live with CCO. We enjoy those so much.
Medical Coding Scenarios & Solutions for E/M
The topic that we’re going to cover this time is Medical Coding and Solutions for E/M. You know, I think E/M, Evaluation and Management, is so much easier than it used to be. It makes more sense to me now and hopefully it does for you as well. We’ll going to dive in and look at some scenarios and solutions. I’m going to simplify it as much as possible. I’m going to come out with a different angle and kind of go through it quickly. But, how you rule out and give some keywords to show you whether it’s going to be level 2,3,4 or 5. We’re going to look at both established and new patients but know that the E/M leveling is the same for those.
E/M Quick Overview
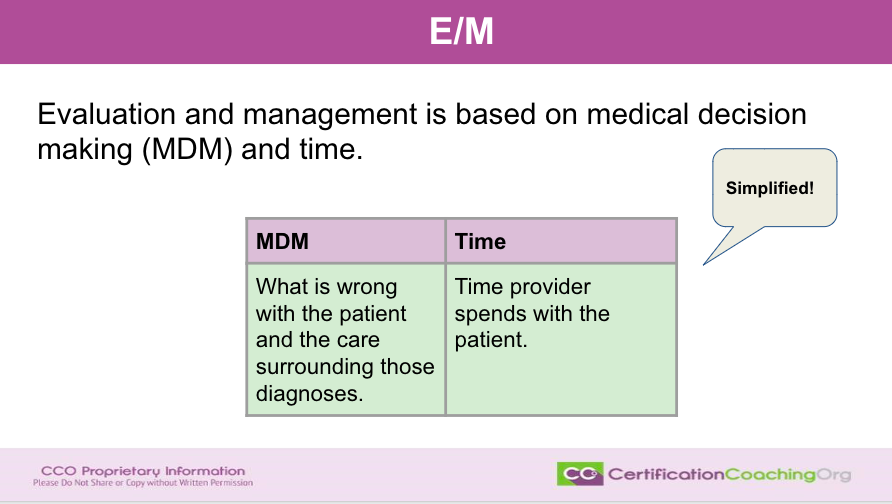
The first thing we’re going to talk about is that, you know, how do we look at E/M now? The E/M is based on time and medical decision making. We’re not going to talk about the time right now. We’re going to focus on medical decision making because quite honestly time is easy. You know, you either spend 10 minutes, 15 minutes, 20 minutes. However, do know that if you say that you spent 30 minutes with the patient as the provider you still have to justify that time. You’re not going to spend 30 minutes with the patient trying to clean serumen out of their ears most likely. You’re not going to get that elevated level unless you can give a reason why and that’s going to be justifiable in most cases. Again, use time. There’s nothing wrong with that but it’s pretty self explanatory. We don’t have to spend a lot of time going over how to level time with E/M.
Medical decision making on the other hand is a little more time consuming but not difficult. We’re going to simplify it by saying, you know, the medical decision making is what’s wrong with the patient and the care surrounding those diagnoses that the patient has. That’s what medical decision making or MDM is based on. Time, the time, the provider spends with the patient. Simplify it. Boil it down to that. There are a lot of other things that we can talk about even if you open up and look at the MDM office matrix or whatever you want to call it. The leveling paperwork and stuff. That can get difficult looking at it. I can just show it really quickly. I use the one for, this one is very, very nice to use. If you want to use Find-A-Code, your encoder may have one as well but they’re all the same exact information. We have a free one on CCO.US. Just go to the freebies and you’ll be able to find it there in the Freebies. Use it as a tool
Hi to everybody that is saying hello. I’m looking forward to talking to you about this subject as well. Again, I use that term. Let’s boil it down. Let’s get to the simplified version of how we do E/M now. What is wrong with the patient, the diagnosis and the care surrounding those diagnosis?
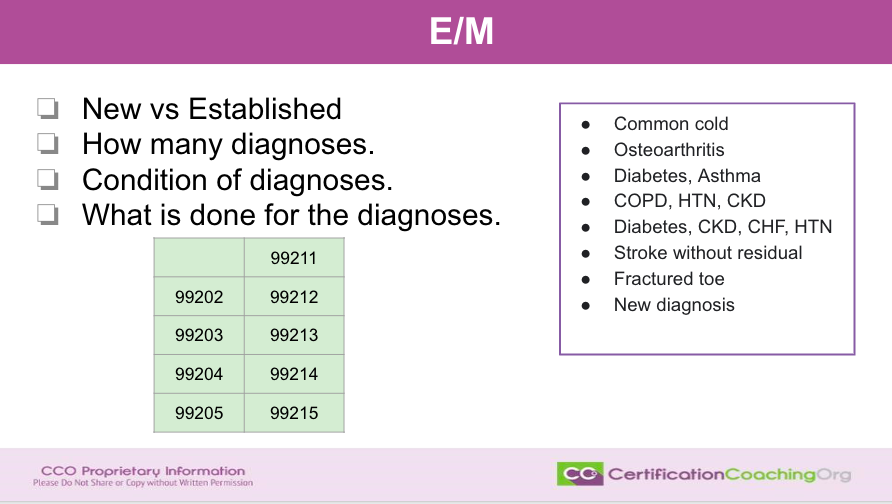
We will be looking at new and established patients. You still divide that up however the leveling is the same. So, you know, yes it is important but when you look at side by side and MDM tools, you’ll see that the 99202 carries the same criteria as 99212 which is an established patient while 99202 is a new patient. One thing after you decide that it’s a new or an established patient, you need to determine how many diagnoses that the patient has. That’s the first step, you know. Does the patient only have one diagnosis, hypertension? Do they have cerumen in the ears, you know, something like that. How many diagnoses the patient has because that will help you determine the medical decision making.
Next, what are the conditions of the diagnosis? And then, last, what’s being done about the diagnosis? These are the questions that you have to ask yourself. If you have a piece of paper, write this down. So, new or established, how many diagnoses, the condition of the diagnosis and what’s being done about the diagnosis. Why do I keep repeating diagnosis? It truly has a lot to do with the diagnosis which tickles me to death now because you know that I love diagnosis coding. And, the way we do E/M makes sense based on medical decision making. How sick is the patient? How many diagnoses has the provider managed and taken care of? Now, we can come up with a lot of scenarios and just to highlight, I listed off some of them and while we were talking I want you to kind of think about it. But we, you know, without having any more content, you know, just off the top of your head, excuse me. If a person has a common cold, what do you think that could level out at this, you know?
Let’s just say we’re working with an established patient, again. What if a person has osteoarthritis or the next patient comes in with diabetes and asthma? What about a patient that comes with COPD, hypertension and CKD? They have three or four diagnoses. Diabetes, CKD, CHF, hypertension. What about a patient that is seen after a stroke without residual or someone fractured a toe or they get a diagnosis? So, these are little scenarios that you can think of off the top of your head and let’s discuss as we move along the disease process that surrounds a list like this. So, we’re not thinking, you know, how many parts of the exam that was done? What was the social history or the family history or personal history that was done? You know, how many body systems did the provider get into? How many tests were done? How many prescriptions were done? You know, we’re going to look at it from a different view point.
Scenario #1 E&M Case Bilateral Otitis Media
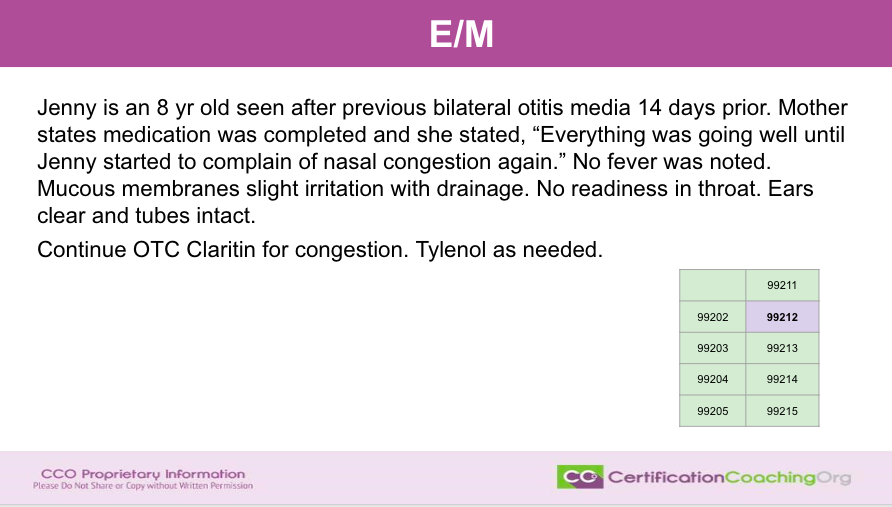
Continue OTC Claritin for congestion. Tylenol as needed.
So, let’s just jump right in. I’m going to tell you that this little grid that I made myself, they’re all green and that this is going to be a 99212. You chat in the comments and let me know if you agree with it but let’s talk about it first. I’m just going to read it out. Jenny is an 8 year old seen after previous bilateral otitis media 14 days prior. Mother stated medication completed and she stated everything was going well until Jenny started to complain nasal congestion again. No fever was noted. Mucous membranes slight irritation with drainage. No redness in throat. Ears clear and tubes intact. Continue over the counter Claritin for congestion. Tylenol as needed.
Now, I’m saying that with the information that was given here. Again, we’re not seeing the whole report and everything. But just in this scenario, I picked it as a level. Do you agree with me and if not why would you think that it’s not a level 2? I’m curious as to what you’re thinking. I am going to talk through my thought process as we go now. The first thing that I want to know is how many diagnoses does the patient have. They really only have one diagnosis. A little nasal congestion, right? And then, the next thing I want to know is what they are doing about it. Well, you know, they looked. They’ve already finished their antibiotics and we know the patient had tubes in her ears but that’s, you know, obviously, they have this routinely and the mother is concerned about it. But, no prescription was given. Direct to use, continue to use over the counter Claritin which is very safe for kids and so this could be a seasonal thing. It doesn’t state that but you know that will help with that drainage and Tylenol over the counter is needed. There’s no fever. No concern. It looks like everybody is agreeing, you know. This is a 99212.
Now, this could have been a full page of information about the past history of the patient having tubes in her ears. Recurrent otitis media in which the patient is 8. They’re probably kind of outgrowing that state. When children, you know, have frequent encounters with otitis media, you know. But overall, really there’s one diagnosis because the otitis media is resolved. You can’t count that. So, what is the one diagnosis? Nasal congestion. The only other thing, overall health patients with very low to you know level straight forward to low medical decision making, go ahead and continue the Claritin and if you need Tylenol, right? So, everybody pretty much agrees with me. Looks like and you know kind of a no brainer there, right? You don’t have to think too hard.
Scenario #2 E&M Case Cut Thumb Laceration
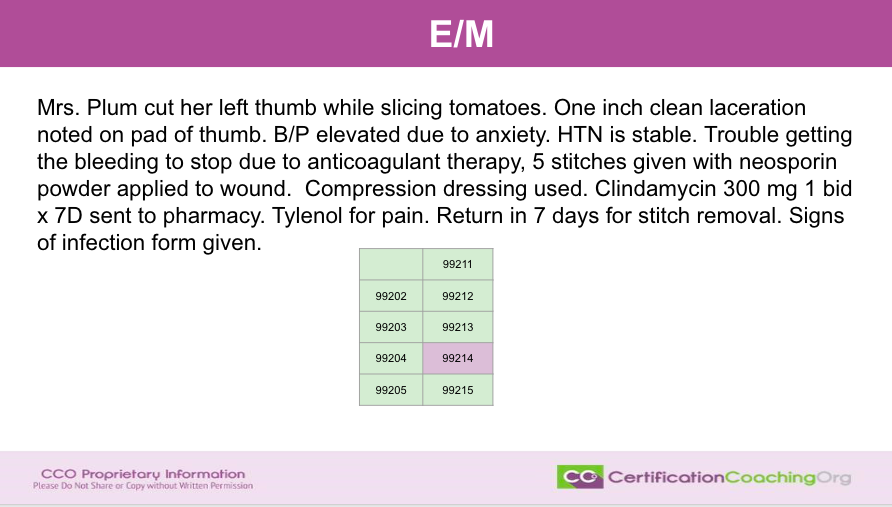
Alright, let’s check the next one. Mrs. Plum cut her right thumb while slicing tomatoes. One inch clean laceration noted on the pad of thumb. Blood pressure elevated due to anxiety. Hypertension is stable. Trouble getting the bleeding to stop due to anticoagulant therapy. Five stitches given with Neosporin powder applied to the wound. Compression dressing used. Clindamycin 300 mg one, twice a day for seven days sent to the pharmacy. Tylenol for pain. Return in seven days for stitch removal. Signs of infection form given.
Jill says would you consider an acute uncomplicated illness over the counter for 99213? Well, I can tell you I’m going to look over at my MDM matrix. And so, you’re saying a, let’s see, an acute uncomplicated illness that would be acute uncomplicated illness would be a 3, correct. But you also have to have two of the three in the medical decision making and if you cannot get two of three you have a number of complexities. That’s acutely uncomplicated. Now, we’re talking about the previous one by the way, guys.
Did we have a review of fibro external notes? Unique source? No. Review test results? No. Ordered test results? No. Assessment requiring an independent historian? You could call the mother maybe an independent historian. You know, maybe. But there would be an amount of complexity in data. I’m going to say no. Then to get to a 3, you have to have a, let’s see. Low risk additional diagnostic testing or treatment. No, none of that was done. So, it would be a 2. You can’t get 2 out of 3 of those levels, Jill. That is why we would decrease that to a 2 versus a 3.
Alright, back to the E/M one. Thank you for asking that Jill. Okay so now we look. Mrs. Plum has a cut on her thumb. Now, when we go to look at something that is going to be considered a level 4 is what I said this one was going to be. With it being a level 4, what are we looking for? First thing we ask ourselves, how many diagnoses did the provider address? Well, we have a laceration. The patient has hypertension and the patient is on anticoagulant therapy. So, we have three diagnoses that the patient is looking at. Now, keep in mind, we don’t have all the other information. We’re basing this so we could say what if or maybe, No, no. We’re basing everything on what we see here. And so, there’s three diagnoses. So, that’s two or more. That’s a little dividing sign on leveling. Two or more. And then, a procedure was performed. That bumps it up automatically. They also gave a prescription. That bumps it up to medical decision making. So when you look at the number of diagnoses, three or more, did the provider have to do any other test or check for anything else? Yup. They didn’t have to do a test but they absolutely did a procedure. They stitched the finger up and they wrote a prescription. So, it bumps it up to a 4. It’s not a three.
Maybe, maybe. A person that had cut their thumb and had stitches, you could say if there was nothing else going on that it could be a three. Okay? But the fact that the patient is on anticoagulant therapy and the patient has hypertension and it’s stable that it was mentioned so therefore you get to count those and that makes the level go up. Yes, Alex you can watch this. Our CCO Lives stay up on Youtube. So, feel free to jump in and watch this again as many times as you need and don’t forget you can go into the Club and ask questions regarding this type of scenario anytime you want.
Alright, anybody disagree with this being a level 4? I’m curious if you would think that that is not a level 4 and the reason that is not a 5 is it’s just not a severe enough complexity, you know. So, as long as everything is stable then you can’t go into a five. You know, five is for really complex patients and this isn’t a complex patient. If there was, you know, something say gosh I don’t know even a cut finger, an autoimmune disorder. They’re going through cancer treatments. They get infections. You know, maybe, you can get into a 5 but again we just have a cut thumb and an inch laceration there on that part of the thumb is pretty significant. However, it…
Is anticoagulant therapy part of the stable chronic problem? Absolutely, it is. Stable and even though they get a little bit, it’s just common knowledge that if you’re on Clonidine then you’re going to bleed more but you know if you read, you know, the rest of the report, they talked about how, you know, they really had trouble getting that to stop bleeding. Well, the only reason that that would be really concerning, I mean, if they were just you know bleeding out and they’re not plus your blood is thinner when you’re on Clonidine. Of course, you’ll bleed more but it also looks horrible. We never understand things that work on clonidine but yeah Isabel that is a stable condition. EDC analyzer also helps us verify level of care. Oh, ok. That’s great. So again, see what we did? How many diagnoses? Were they stable, chronic, complex and what did the provider have to do about it? Very good. Let’s jump over to the next one.
Scenario #3 E&M Case Fracture Left Wrist
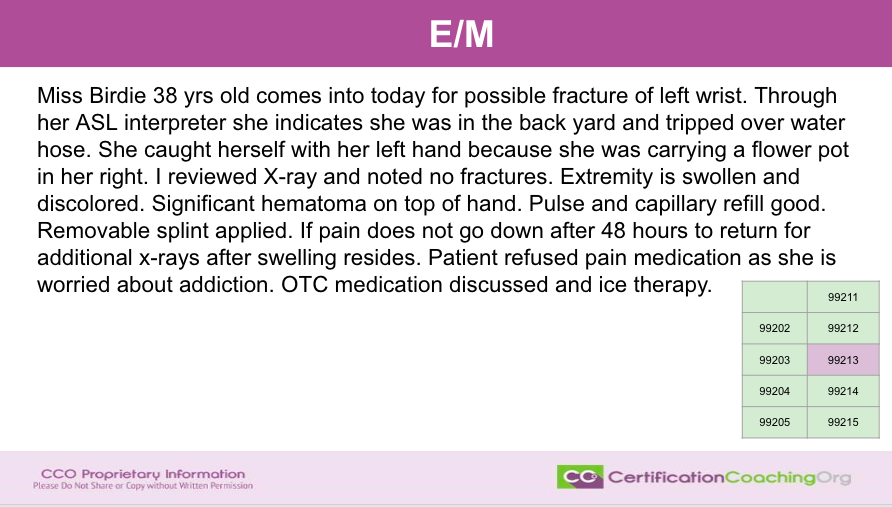
So, a few things that trick people up when they’re new to E/M. They start reading into the possibilities. The fact that the patient has an interpreter, that makes some people say oh well they’re independent historians. They could, you know, no. Do not consider. An interpreter is not, an ASL interpreter for American sign language, Brenda. So, this patient is deaf. Well, just because they’re deaf is not an additional diagnosis. Just because they have an interpreter doesn’t mean that they need an independent historian. When a patient has a translator, it makes them one. So, you cannot use that as, meaning, you know an independent historian and that’s why I picked this. I wanted to see if any of you guys thought oh wait, no, no. Don’t they get something for that? No, no. They’re one and the same person when that happens. Also, the fact that the provider was going to write a prescription, so the intent was there but the patient refused. So, does the provider get credit for wanting to write the prescription and the patient not. You know, the intent was to write a prescription so they get a point you know a level for that? No, they don’t. The patient said no so they didn’t have to do that. They didn’t have to think about what medication to give her. And if it counteracted with anything else they were taking.
So again, we can’t bump up with that either and there’s nothing here that would allow us to go from a three to a four. One diagnosis. Diagnosis, it’s acute but it’s not complicated. Sometimes, they’ll say oh you know, a hematoma, swelling. There’s something else going on. Capillary refills in the pulses and pulses are all good. Stable. No, it is not complex. They have sprained their wrists. So, very good. This would be a three and all of the information that is above and beyond that about you know how it happened. They tripped. They’re carrying flower pots, blah, blah, blah. That’s fotter. That really doesn’t apply. Now, it does apply if you’re grabbing diagnosis codes. You know, that’s different but you know it does not apply as far as the medical decision making for what’s going on with this patient.
I can tell you for those of you out there that are students that are trying to understand E/M, really narrow focus on how many diagnoses the patient has, how complex the diagnosis and then number 3, what is the provider going to do about it. So, we’ve answered those in this scenario. Let’s move on to the next one.
Scenario #4 E&M Case Pain in Fingers and Wrists
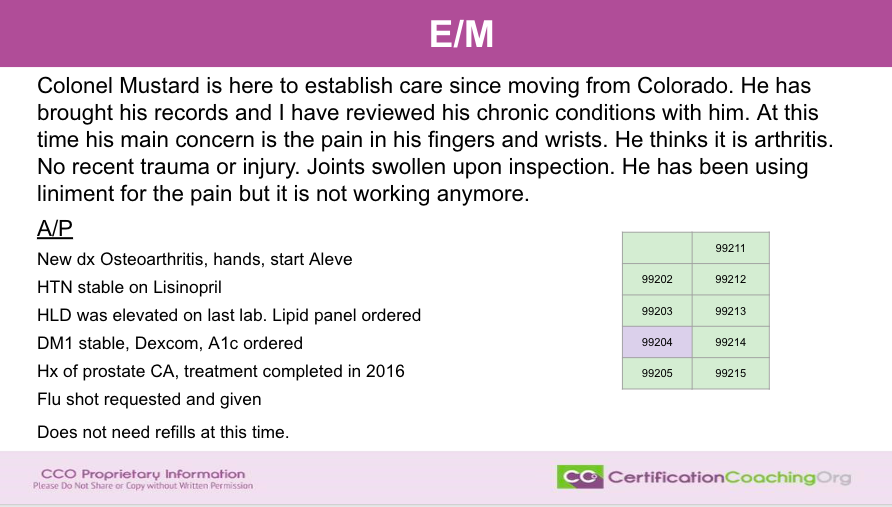
Alright. Now, we have Colonel Mustard. Do you get a thing over here? Do you guys recognize these names that I use sometimes? Colonel Mustard? Mrs. Plum? If you guys know whom I’m referencing, put it in there. Let’s see. Isabel says, if the patient accepted the prescription, we could use four, right? Yeah, you could. You could bump it up with the four. That is, Isabel, a good point. Yeah, clue. Brenda, Yvonne, Tiffany, you guys got it. It’s really hard to come up with names when you reduce stuff and when you’re making up scenarios. So, to be able to pull something from like a clue, one of my favorite movies, I watched it again not too long ago.
Alright, Colonel Mustard is here to establish care since moving from Colorado. He has brought his records and I have reviewed his chronic conditions with him. At this time, his main concern is the pain in his fingers and wrists. He thinks it is arthritis. No recent trauma or injury. Joints swollen upon inspection. He has been using liniment for the pain but it is not working anymore and so that’s the main HMP then diagnoses that are reviewed. New diagnosis of osteoarthritis in the hands, start Aleve, which is over the counter. Let’s see, hypertension is stable on Lisinopril. Hyperlipidemia was elevated in the last lab that he reviewed. Lipid panel ordered. Type 1 Diabetes, stable. He has Dexcom which is one of those things you put in on your arm that you can check your blood sugar on your phone. A1C has been ordered. History of prostate cancer treatment completed in 2016. Brilliant documentation by the provider. Flu shot requested and given. Does not need refills at this time. So, you know, he recently moved in from another state. And that, he’s got current refills, you know, probably transferred his refills. He has established care so when it’s time, he’ll be able to go and get refills again.
So, what are our questions we have to ask ourselves? How many diagnoses is the provider looking at? So, we have 1, osteoarthritis, hypertension, hyperlipidemia, diabetes and history of prostate cancer. Now, you said wait, history of prostate cancer is not a current diagnosis. The fact is that he reviewed the information about prostate cancer and saw that it was in the past but that also is part of, let’s see, medical decision making. This patient has had prostate cancer in the past. It was in 2016. He will continue to check for malignancies and metastases and other conditions that could become problematic after having had cancer. So, that does, you know, include. So, we have one, two, three, four, five. Five diagnoses that we have on there. Alex says, quick question. Do referrals to a specialist or referral to a podiatry count towards a medical decision making? Yes, it does. It absolutely does. Specialist referring to a specialist stating why this particular one could say, you know, history of prostate cancer of the patient still had concerns then referral to your neurologist. Yeah.
Yvonne says, oops, I missed the prostate cancer step. Yeah. Five things. Some people would say well you don’t have to count the prostate cancer, Yvonne, because it’s in the past. The fact is the provider reviewed that history is a diagnosis and it states that the treatment was completed in 2016 but they still are considering it as part of their medical decision making. So, very very good. Alright, we have five diagnoses. What are they doing about it? Or wait. Complexity, we’ll do complexity next. We have a new diagnosis. That bumps the complexity up. We have ordered tests, two tests. Lipid panel and A1C. They also gave a flu shot which that would be modifier, you know, on there and as a procedure and stuff. Again, that is still something else that was done is that the provider has to look and say oh okay, you haven’t had your flu shot. Yes, we can provide that for you here. But that is not a diagnosis. That’s something you’re doing to the patient. Again, how complex is whenever you have a new diagnosis, that bumps that the complexity up.
Now, if we had 5 diagnoses that they were managing and all of them are stable and no prescriptions were being, you know, that still bumps it up because you go in and look, let’s see, even if a three, it would be two or more self limited or miner, you know. So, when you get into, it would be a four with two plus stable chronic illnesses. So, we have five but we have four that we are going to say is they’re not stable. The hypertension is stable. That’s one and the diabetes is stable but he orders an A1C, okay? But he did state it was stable. Two stable diagnoses and I’m not going to count the prostate cancer as stable because we’re going to take that away. But they have a new diagnosis that bumps it up and we ordered labs because the hyperlipidemia was elevated and so therefore, we’re ordering a test. So, what did they do with that one over the counter medication? Now, we’re going to the next step. So what is the doctor going to do about it? We’ve ordered two tests. So can’t get in to a high, you can’t get in to a five because there is no emergency here. Pretty much. Everything is relatively stable and what’s not is not complex.
So, Isabel says, if the doctor didn’t ask further about the history of cancer, would that still be coded? No, you’re going to code it, period. No, no, no. Let me rephrase that. If the doctor didn’t ask further about the history, the fact that is stated in the documentation, it would be coded, okay? Now, don’t get confused. You know, there’s risk adjustment. You would code it absolutely. You would count it but the fact that it was stated and in the assessment and plan, it gets coded. He had to think about it. So, absolutely we’re at a four. We’re above three because we have 5. We ordered tests. One is a new diagnosis. One is elevated so it’s not stable, right? But nothing is really complex. Just ordering tests to see where they’re at. Okay? Alright. Let’s see what we got next.
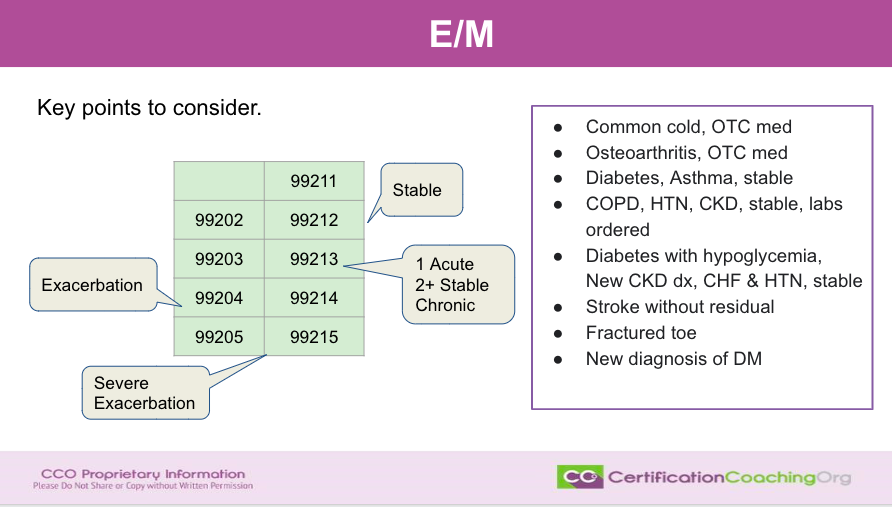
We’re going to talk about the key components. What I wanted to do is kind of give you shout out phrases. If everything is stable, you’re a 2 and maybe a three. If you have an exacerbation of anything, you’re probably going to be a 4. If you have one acute and two stable chronic conditions, it’s a three. If you have severe exacerbation, it’s a five, right? So these are just little takeaways that you can use to tell yourself. So, what are the key things to consider? The first thing is how many diagnoses. The second thing, the complexity of those diagnoses. The third thing is what are they doing about it. How complex or what do we have to do about it? Those key phrases and statements. You’ll be looking for stable. If there are acute and you can have acute but you don’t want multiple acute. If you have multiple acute, new diagnoses then that bumps it up to a four. But if you have even one acute and two or more stable, that’s still a three if it’s not complex. But if you ever see exacerbation written anywhere, that automatically bumps you up to a four. Okay?
So, let’s talk about this box here. Let’s go back to the ones that we were talking about and let’s kind of work through them in our heads. So if you have a common cold and the treatment is over the counter medication, what do you think you’re going to be? Note that it’s going to be, it’s not going to be a five. It’s not going to be a four. Is it going to be a three, two or one? Does anybody want to shout it out? Would they think so? Yup. Brenda says two. She nailed it. Yeah, it’s going to be a two. Common? No, it’s not complex. Yup, everybody is nailing it now. Right, a two. One thing and it’s not complex and the medical decision making is not complex. So, it’s a two. Not a three, Suzette. Why, let me know why you think it might be a three? Because I want to know what your thought process is. Maybe you’re thinking of something that I’m not seeing. Vanessa, why do you think it’s a three and not a two? Let me know so that I can make sure we’re on the same thing. Maybe I’m missing something. While I’m doing that, I’ll take a sippy, sippy here. So, I don’t have a sneezing fit.
I’m curious as to what a common cold is with over the counter meds. So, how many diagnoses do we have? One. What’s the complexity of it? Very low because it is just over the counter medication. What’s medical, you know, what are they doing about it? They’re not doing anything about it. So, Alex says, if they did a respiratory panel, wouldn’t it bump it to a level 3? Yes, it would. If they did a nebulizer treatment, it would bump it up to a three. But the way it is now with only we knowing that it’s a cold and over the counter, it’s a two. Tell me what you’re thinking about Suzette and Vanessa and let me know so that, so we’ll move on to the next one. I know you may be typing a lot.
Okay, next one, oh I’m over assuming. Possibly. Yeah, I see what you’re thinking. You’re just thinking through the process. Got it. Osteoarthritis, over the counter medication. So, we know it’s not a five. We know it’s not a four. Is it a three or a two? Oh, Yolanda says, why won’t it be a 1? Well, a 1, you’re not even really seeing the provider. So, they actually saw the provider so there are two. Good question though Yolanda. Very good question. But with the 1, it’s one self limited or minor amount of complexity, none or minimal. Risk for diagnosing straightforward? They, let’s see, examples that they used for low if that would be a 3 would be well controlled hypertension, not insulin diabetes, cataract, benign prostate hyperplasia. It is acute. It’s one acute uncomplicated injury or illness. So, an acute cold is acute. Yup, Yolanda, you’re seeing a nurse with that one. Vanessa, let’s see. Oh, oh. We’re on the next one.
Osteoarthritis, over the counter medication. In the past, if they saw the nurse have stitches removed, that’s a one. If they want their blood pressure checked, that’s a one. Review of their blood pressure, that would be a 1. Yeah, good question Isabel. Osteoarthritis over the counter meds, everybody is saying that it’s a three. I’m thinking that it is still a two. Tell me what’s the difference in the common cold – over the counter medication and osteoarthritis with over the counter medication is? What would be different except one is acute and one is a stable chronic? So, that would still be a three and then low risk. So, I’m thinking that osteoarthritis with over the counter medication would still be a two. What do you guys think? Do you still think it would be a three? Still one diagnosis and over the counter. Brenda, that’s what my thinking is, too. I thought osteoarthritis would be considered as stable chronic. It is a stable chronic and that is 99213. If you can get two of the three. So, we have stable chronic and it’s well controlled. So, we would get a two. Yup. Now, if the patient has osteoarthritis and was having a flare then maybe you could bump it up, you know, stuff like that or what if they had osteoarthritis and the provider was saying you know what this may not be osteoarthritis. This is starting to look like rheumatoid arthritis. Let’s do run some blood work. That bumps it up to a three.
Alright, diabetes, asthma. Diabetes and asthma stable, what are we thinking? It’s not a five. It’s not a two. It’s either a three or a four. Diabetes and asthma stable? Okay, this one is a little more complicated because we are not given any information that a prescription was done. We don’t know if any tests were reviewed or anything was ordered. It is true that if you look at the leveling thing, two or more stable chronic illnesses, okay, but you can’t, you are going to meet two of the three things. So, how many diagnoses? We have two. Oh, okay. That could mean a three or a four. And then, how complex are they? Well, not complex. Do you think diabetes is complex? Well, it is but it’s stable and we’re not getting a prescription. We don’t know anything else so that is low. What’s the doctor going to do about it? Nothing. So, we cannot be a four because we have to meet three. We have to meet two of the three and we can only meet one of the three. You have to meet or exceed the criteria in the column. How many diagnoses? Two. Okay. So, that would be a three or a four. Are they complex? No. They’re chronic but they’re stable. And, did the doctor do anything about it? No. So, you have to make two, you have to have two or three and still have, let see, two self limited or minor one stable chronic or/and well controlled because they’re stable. No, you’re going to get a three. You can’t get a four out of it. Kind of cool.
Hi. Oh, Stevangie, I don’t know if I pronounce your name. I’m glad that you’re here. Alright, question. Do you think over the counter medications recommendations counters prescription management? No. I don’t. So, the scenario would be to think of cerumen in the ears and the provider says hey go get them, they sometimes tell them to put stool softeners in their ears and then Isabel says I’m confused. Okay, remember they got to get two of the three in the column. So, you’re writing to your three columns there. Three things you have to ask yourself and you’ve got to be able to get two of those fingers to be able to go to the next level. So it’s MEAT or seek exceed.
But let’s try another one. Okay. So let’s go to COPD, hypertension, CKD are stable labs ordered. What do you think that is? That’s a 4. Why? Two or more chronic diseases. How many chronic conditions? We have three chronic conditions. They’re stable. Okay, so what so, you know, are they complex? No, they’re not complex, but they ordered tests. So now, you have two of the three and you can get into a four. They’re not ordered tests. It would still be a three. But they ordered labs. So that it automatically lets us bump up. Now again, we’re really making this kind of, you know, there’s other scenarios. Don’t tell yourself. What if, only think about what information you’re given.
Let’s go on. Next one, diabetes with hypoglycemia. That is how many diagnoses? One. Is it complex? Yes. It’s complex. It’s diabetes and it’s having complications, hypoglycemia. Doesn’t say what they’re going to do about it. But, you’ve already met two of the three. Two of the three so that’s a four. That would be the equivalent of saying there’s an exacerbation to diabetes. So, how many diagnoses? One. Okay. It’s chronic, but it’s complex because it’s a complication. What are they going to do about it? Well, we don’t know so we can’t count that. But if we know that they would order a test, but still that becomes a four.
Next one. New CKD diagnosis, CHF and hypertension stable. Oh wait, that was on the other bullet. Okay. Sorry, let’s go back up. Diabetes with hypoglycemia, new CKD diagnosis, CHF and hypertension stable. Oh, sorry. I didn’t see that. I thought that was another bullet with the new diagnosis. So, we have now how many diagnoses? One, two, three, four. Four diagnoses. You have two of them with higher complexity because one’s new and one’s got a complication and two are stable. So, that gives you four diagnoses. Now, you cannot get into a five and let me tell you why because they’re not showing you what they did about it, but for it to be a five you need one chronic illness with severe exacerbation.
Progression or side effect of treatment or one acute or chronic illness posing threat to life or bodily function. We’re not there yet. However on a four, you have two plus stable. Yes, but you’ve got an undiagnosed new problem with uncertain prognosis, new CKD. You have a diabetic that’s now a CKD patient that is elevating. That’s a complexity of diabetes plus hypoglycemia plus CHF and hypertension to get together. So really, um, I would not classify that as a I wouldn’t I wouldn’t say that’s an exacerbation. I would say the complexity is higher. So, I would still rate that as a four. Yolanda says a five. Now, if we knew what tests were being done, the fact that they’re not here is kind of bad. But, you know, absolutely if they had referred to renal and with diabetes, the hypoglycemia referred to endocrine and again, I’m going through these with the prospect that these are all family practices and stuff.
So, Yolanda’s thinking of five. I’m going to still say it’s a four because it’s not a very exacerbation. It’s hypoglycemia, but it is a new diagnosis. And so, it says one, let’s see, one chronic illness exacerbated and two stable chronic illnesses under, let’s see under diagnosed new problem with uncertain prognosis not you know, so still those fall in the four. Yeah, so I would go with a four. If we had all of the information we knew what they were doing with the then we could probably maybe get it into a five but I would say most likely not we’re still probably at a four.
All right. What about strokes without residual? What do you guys think about that? Stroke without a residual means no side effects. Yep, Miley says a three. I agree. It’s a three and the reason I would say it’s a three, Yvonne, I know you said two and the reason I would say it’s not a two is that when a person has a stroke or has had a stroke, if this is the visit for after the stroke the doctor is going to be looking at a lot of documentation and reports about the stroke and making medical decision making goes up because obviously this patient’s going to be put on medications. They’re probably going to be on anticoagulant therapy now and stuff so they’re gonna be a three, not a two but if they had anything else going on then we might bump them up to a four but I could tell you that it’s going to be a three and then they reviewed prior external notes from unique sources, review of tests. All of that is two.
So, how many diagnoses? One. How complex? It’s not complex. But what does the provider do about it? They had to read a lot of documentation if it’s a follow-up of a recent stroke, even though there was no residual. Now, even if it’s stable. Yes Yvonne because we and again we’re making an assumption here without the note but we know that if we set the scenario that this is a patient that comes in and sees their provider after the stroke and they have no residual they’re doing fine, that provider is going to spend a lot of time reviewing that record. The patient’s records and talking to them and educating them. However, now Yvonne how it might be a two is if the patient is just coming in for whatever they’ve not they don’t have anything else gone. The previous stroke was six months ago and that’s all that’s wrong with the patient. There’s nothing else wrong with the patient. That would be it two.
Okay, so let’s say with the information we’re given probably a two because with your thought process. My thought process is okay if this is the first visit after a stroke, it’s going to be a three. So again, we could be both right. Hopefully that being said, it helps you to determine what you need to think about when you see these scenarios. Okay. Yvonne makes another point depending on the length of time since the stroke makes sense and how long they spend the time with the patient. This might be a scenario where they do it based on time and not medical decision making because not only do they review the notes, but they have to educate the patient and answer all their questions about, hey, I had a stroke am I going to have another one and you know, is this gonna kill me? Is this gonna you know, what do I need to look for? What is a residual? What are late effects? What are all these words that I heard? So in this scenario in the real world if that’s all that was going on. The provider would probably base it on time, not medical decision making. Let’s see for, yeah, time spent with documents. Yeah Cindy time spent documented and stuff. So you have to have the time documented for them to use that. Yep.
All right, so, let’s see the fractured toe. What do you think about a fractured toe? Let’s give you more scenarios. Let’s say it was a 17 year old male football player and he was goofing around and tried to kick the ball, try to get a field goal and practice without his shoes on and he broke his big toe. What do you think that would be? So how many diagnoses? One. Is it complex? Well, yes. It’s complex because you’ve got to do something about a fractured toe. Now, usually they’ll just tape them together. However, again how many times now do they send them off to and or the pit is to go look at it, right? If he’s a football player and he’s healthy and stuff maybe they may just but they did an x-ray or they wouldn’t know that it was a fractured toe. So yeah, we’re looking at a three for him and now let’s change it up.
Let’s assume something here. Just real quick. What if this is a 75 year old that got up in the middle of the night to go to the bathroom because they have prostate cancer and they pee all the time and they’re also a diabetic and they broke their toe? That is going to change the leveling, right? So, the fact that we don’t have any more information we can only make assumptions but if you have a fractured toe, you know that you’re going to be a three or four out the gate right because tests are being done and stuff like that and most likely it’s a four because they’re going to do an x-ray. You’re right. They’re gonna give them pain medication, you know, and we’re making a lot of assumptions but anytime there’s a fracture that elevates the complexity and what the providers are going to do about it. So, keep that in mind.
And last, we’ll say a new diagnosis of diabetes in a patient. The new diagnosis of diabetes elevates, right? It is complex whether they’re going to treat it with medication or diet or exercise or so. So with a new diagnosis. Let’s see. We are looking at one undiagnosed new problem with uncertain prognosis. That’s what I would say at a four and I would say you’re tipping three and four, but probably a four right because diabetes is a diagnosis that is just more complex. Now, if it’s a new diagnosis of hypertension, three probably and again, we’re just thinking kind of on the medical field, your background knowledge of what it is. A new diagnosis of diabetes, hey, that takes a lot of education. That takes a lot of thought processes of you know, what are we going to do? Are we going to do diet and exercise? Do we need to go ahead and start you on medication, you know, family history plays a part there. How fat you are, we don’t have that information.
But I’m saying probably you’re going to get a four out of that if you have the rest of the notes because diabetes is a complex diagnosis, especially when it’s new. Because what if I said a new diagnosis of Alzheimer’s? Will your brain automatically thinks all four four, right? So again think of it that way and again Cindy makes a good point. Time might be a factor there because a lot of education, a lot of reviewing of labs that were probably taking you can’t give them a new diagnosis of diabetes without having had labs done in reviewing those laps. So again, we’re probably looking at a four regardless. I hope guys that this kind of overview of thought process is how you look at E&M versus, oh my gosh, there’s a leveler and I’ve got a check and count all this stuff kind of think of it as you can’t use information that’s not in the documentation.
Now I’ve kind of made light of this and this is kind of remedial in a lot of ways. We’re making a lot of assumptions and stuff but always remember you have to go down to the basics. Three things. One. How many diagnoses? How complex are they? And what’s the provider going to do about it? Ask yourself those three things and when you do that, that’s the three columns, right? And you should be able to kind of think that through just two of those. You have to have two of those or you have to have multiple diagnoses. It has to be complex diagnoses or you have to be doing something about a lot of things about it. Okay?
Submit Your Topic Requests
We’re gonna wrap up guys. If you have a topic you would like us to go over and kind of unpack it like we did tonight give scenarios, examples, walk through it kind of do something live like this. Absolutely. Let us know the topic you would like us to cover at CCO.us/topic-request. We look at your requests. We always look at our students first, then we look at the club members and look at their requests and then all of the outsiders that send topic requests and if you want to be top of the list then again, you can become a student with us. If you like the way that we educate, this is the way we do it across the board with the other credentials. Go to cco.us. Look at our courses. We have a great course on risk adjustment and medical coding.
We also have a lot of products that just help you pass the tests, the credentialing exams, but we also have our fabulous CCO Club – CCO.us/club where we have discussions like this and there’s lots of exclusive content in there and videos like this that might be helpful to you and it’s a nominal cost every month. Again, I hope you had fun. We have fun doing this. We really appreciate when you join us and feel free to share and let other people know about us. We really don’t advertise and we would appreciate getting the word out if this was helpful to you. CCO.us, don’t forget that and if you’re on whichever social media that you’re using you can splash it out there. Share it. Tell other people about us and you guys have fun coding. Have fun learning. We have fun educating. Thanks guys. Bye.

![[CCO] Certification Coaching Organization LLC [CCO] Certification Coaching Organization LLC](https://www.cco.us/wp-content/uploads/2015/05/CCO-Logo-2015-d3-500px.png)